Life at Home
Sunday, March 13, 2016
Home stretch. (This is what I keep chanting in my head). We are in the home stretch. Tucker is still inpatient on the pediatric floor but has made significant progress towards discharge. They were able to remove his Foley catheter yesterday and he’s been going to the bathroom on his own – yay! We have modified his G-tube feeds to a lower, continuous rate, but we know that as his GI system continues to wake back up, we will transition back to his usual diet.
Earlier today, they took his last (of four!) peripheral IVs out of his foot this morning which is nice, because Tucker basically hasn’t walked in over a week. He’s definitely got sea legs and is a little wobbly walking. We anticipate that this will go away once we get home and he can continue his usual level of activity.
At this point, the only thing keeping Tucker in the hospital is the weaning of his sedation meds. The pain management team will give his final dose of Ativan tomorrow morning, and then they will want to watch him for a few more hours to make sure there are no significant withdrawal symptoms. If all looks good, they will discharge us Monday evening or Tuesday morning.
I rebooked our flights back to Richmond for noon on Tuesday. We are ready!
Friday, March 11, 2016
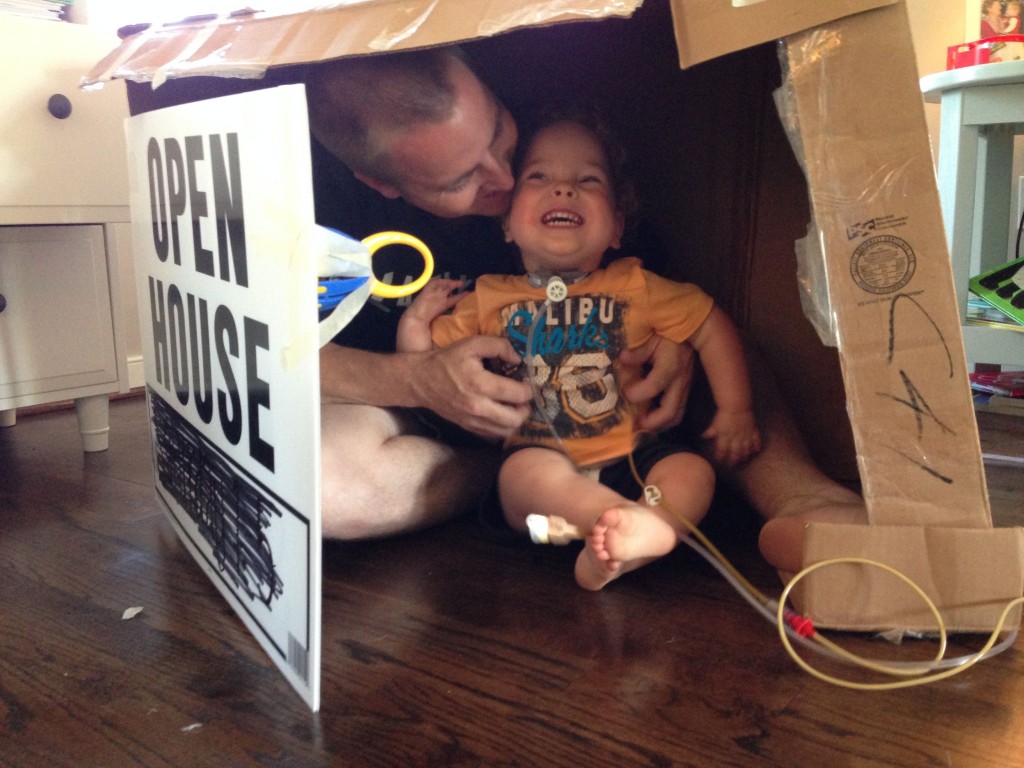
We came full circle when the same surgeon who performed Tucker’s tracheostomy in April 2013 returned from the OR yesterday with the news that Tucker’s surgical site looks beautiful, and Tucker’s trach is gone.
We held this news close with cautious enthusiasm, wanting to give Tucker a little breathing room to prove he could fly. We thought for sure, after a major surgery and a week of heavy narcotics, Tucker’s ENT would put his trach back in (temporarily) to get him over the hump of recovery. We had already begun discussing our return trip in April to decannulate. Never one to disappoint, Tucker surprised us all.
To those you who prayed boldly and courageously that this trip would be the final stage of our trach journey, thank you. We were floored when first saw him back from the OR, with a naked neck and holding his own. This is a game changer for our family in ways we don’t even realize yet. He’s doing great so far, and looking and acting more and more like himself.
Since Tucker is doing well and no longer requires ICU level care, they will transition him to the pediatric floor later today, where he will stay until it’s time for him to discharge. Right now, it’s looking like Tucker will be discharged on Tuesday or Wednesday of next week. We still have a few things to check off the list before it’s safe for Tucker to come home, and if you would like to join our family in praying for these things, that would be wonderful!
- Tucker’s GI motility is still slow and he’s having difficult using the bathroom on his own without medical intervention. Pray that he will poop and pee.
- Pray that Tucker’s stomach will wake up and start tolerating tube feedings.
- Tucker needs to wean down off of the narcotics he has been on over the last week. Yesterday was certainly his worst day of withdrawal, and now that we are through the worst of it, we are hopeful we can wean him off the meds by the beginning of next week.
We are so very excited. What a week.
Wednesday, March 9, 20161
We are on Day 6 of sedation and as you can imagine, we are pretty weary and ready to get our boy back. It has been a long six days. Fortunately, this is the last day of this part in the process. Tomorrow, Tucker goes back to the OR for a bronch of his airway to see how everything is healing up. We are anxious to see how his surgical site looks. We are even more eager to know next steps.
A few prayer requests and answers to prayers:
- Patient/family hospital housing was able to extend our reservation through Tuesday, March 15th – giving us an extra five days beyond what they originally offered us. This is great news and a direct answer to prayer. Thank you!
- Pray for Tucker as he wakes up from all of these medications. I am not sure which is worse, watching your toddler sedated and intubated for a week, or watching your toddler go through withdrawals from morphine and medazolam. Either way, we are buckling up for a hard weekend as they start titrating his medications back down. Pray for the weaning process to go (relatively) smoothly.
-Pray for Tucker’s GI motility. He is on day six without any kind of significant nutrition because he currently is not tolerating feedings through his G-tube. Everything is just backing up and not moving through. In basic terms, pray for this kid to poop so they we can start feeding him real food. It will be crucial to his recovery.
We will post again tomorrow with the results of his bronch, and about next steps and plans for his trach.
Monday, March 7, 2016
Tucker had a relatively quiet weekend. He remains sedated post-operatively so that the surgical site around his trachea can heal. It took the first 24 hours after surgery to titrate Tucker’s IV medications to capture him. (Unfortunately, when you are a 3-year-old boy who is busy and has lots energy, and you’ve had a medical history where your body has already seen a fair amount of these drugs before), it takes a little while to figure out the right cocktail of medications to keep you still.
We’ve been fortunate to have several nurses who have taken care of Tucker in the past assigned to him again during his recovery. It’s always nice to see a familiar face who knows your kid.
Some specific things you could pray for:
- Nutrition for Tucker. Currently, several of the medications Tucker is on slow down his digestive motility. Meaning things aren’t moving through as and should, and he isn’t tolerating any food through him G-tube (it’s just sitting in his belly). While this is not dangerous at this point, it would be beneficial to get him some good nutrition as he continues to heal.
- Patience for Tommy and Ellie. We have been through a similar post-op recovery process two years ago with Tucker’s esophageal atresia repair. Although that sedation period was longer when he was an infant, we’ve certainly “missed” the presence of his little personality a whole lot more this time around. Pray that we can hang in there until Thursday, when he returns to the OR of a scope of his newly repaired airway.
- Decision-time on Thursday as to whether or not we should re-insert Tucker’s trach. This depends a lot up Tucker’s lungs and whether Tucker’s ENT feels safe putting him on a plane and sending us home, trach-less. We are really fine either way, and the great news is that even if they re-insert the trach on Thursday, it will be temporary to get us “over the hump” over Tucker’s recovery. We would return mid-April to decannulate permanently if Dr. Nuss decides to re-trach.
March 4, 2016 (Will be updated throughout the day)
*1:30 pm. Tucker is out of surgery. Everything went smoothly and Tucker was stable throughout. Dr. Nuss (Tucker’s ENT) had a great team of anesthesiologists helping managing Tucker’s lungs and respiratory status so that he could focus on repairing Tucker’s airway.
Dr. Nuss removed about 17-18 mm of “bad cartilage” where Tucker’s trach had caused his airway to become floppy (making it difficult for him to breathe). He replaced that area with a rib graft.
Tucker is intubated nasally and will remain quiet and sedate for the next three days. It’s crucial that his airway have time to heal and stabilize so that Tucker can receive the long-term benefit of this surgery. Dr. Nuss said that the ICU will begin to lift the sedation medications after three days so that Tucker is still quiet, but a little bit more alert and present.
Tucker will go back to the OR next Thursday, March 10th (six days from now) for another scope of his airway. At this point, Dr. Nuss and his team will evaluate both Tucker’s lungs and his airway to determine whether to re-insert Tucker’s trach temporarily (about six weeks), or keep the trach out and we go home trach-free. How Tucker’s lungs handle the sedation and mechanical ventilation over the next several days will influence this decision. Either way, we are trusting the Lord knows what is best for Tucker and will make that clear to his medical team.
We are excited for Tucker and thankful for a smooth surgery. We will continue to update while we are in Boston.
**12:00 pm: The airway reconstruction is going well and Tucker is stable.
**10:30 am: Rib graft is finished and tracheal reconstruction has begun.
**8:55 am: I just got a call from his nurse in the OR that all of his IV lines are in, he’s prepped, and they are about to begin surgery.
Tucker went back to the OR this morning for his tracheal reconstruction around 7:45 am. The doctor told us that we can anticipate Tucker will be in the OR for 5-6 hours. They will call out every 1 1/2 hours with an update on how things are going.
Thanks for praying for our buddy! This is a big surgery and we don’t take your prayers or support for granted. They carry us through. ![]()
February 28, 2016
It’s been awhile….We are headed to Boston this Thursday, March 3rd for Part 1 of a two-part reconstructive surgery for Tucker. We are still learning more about this surgery and what it entails. Here’s what we know so far:
- Tucker has what’s referred to as “suprastomal collapse.” Meaning, he has had a trach in long enough that the muscles in his airway have atrophied from the trach “stenting” his airway open.
- This problem is corrected surgically by grafting a piece of cartilage from Tucker’s rib and reinforcing the area of his airway where there is “collapse.”
- The first and most intense part of this repair will take place this Friday, March 4th. Tucker is scheduled as the first case in the OR at 7:30 am.
- He should be in the operating room for 4-5 hours while his surgeon repairs his airway.
- Tucker’s ENT will temporarily remove his trach to let the repair site heal. Instead, he will remained intubated by mouth and sedated for six days as the site continues to heal.
- Tucker will go back to the OR on Thursday, March 10th for a bronchoscopy and trach re-insertion. This is Stage 2 of this repair. The trach will remain in place for several more months until we return to Boston this summer to permanently remove it.
- Tucker will likely require another 3-4 days in the ICU after his trach is put back in place to wean the pain and sedation medications he will have been on for the last week.
- At this point, we are planning to be in Boston for about two weeks.
July 5, 2015
Well, I think it’s safe to say the outcome of this holiday weekend is not quite what we expected. Probably the first Fourth of July where we were both in bed by 9 pm and all three of us slept through the July 4th fireworks. We are enjoying a slow, rainy Sunday morning back at home, but here is a recap of what went down for those who have followed along.
Tucker went in for a routine decannulation (trach removal) trial on Friday. The game plan was to admit Tucker directly to the children’s intensive care unit on Friday morning, pull out his tracheostomy, observe him and keep him overnight, and send him home 24 hours later with a band-aid on his neck.
Tucker did great initially after we pulled the trach out on Friday morning. His oxygen saturations were beautiful, he was talking, playing, and breathing comfortably. We spent a good portion of the day in the Children’s garden outside the hospital unit. We went into the evening feeling excited and celebratory, as most of you did on social media, that this was the end of one chapter and beginning of another.
Things took a turn on Friday night shortly after Tucker fell asleep. He quickly developed an audible stridor (noisy breathing) which typically indicates a floppy airway. I could attach the audio bite we took of his stridor Friday night, but I think we would scare people.
We also noticed retractions throughout his abdomen and ribcage, evidence that Tucker experienced difficulty taking good breaths. We gave him some blow-by oxygen throughout the night, which helped him a little, but he still had a significant stridor and restless sleep pattern.
His ENT took him to the OR Saturday morning for a repeat direct laryngoscopy bronchoscopy to examine his upper airway without the trach in. The anesthesiologist simulated a sleep-like state while Tucker was under, and Tucker’s ENT said the stridor and retracted breathing began almost immediately.
What she found when she was down there was significant tracheal collapse above his trach site and below the larynx. Meaning, when Tucker is awake, his muscles are taut and he is stinting his own airway open. When he’s asleep and his muscles relax, the muscles around his trachea flop closed, preventing him from getting good air supply.
What we didn’t realize prior to all of this was, he was solely relying on his trach to keep his airway open at night. With the trach out, we now had a clear picture of Tucker’s upper airway collapse.
The medical term for this is “suprastomal collapse” and ironically, it’s a condition caused by long-term use of the trach itself. Because Tucker has been trach-ed for 2+ years now, the muscles and cartilage in his trachea above his trach have atrophied. Since they haven’t needed to work for so long, they’ve lost their rigidness.
Unfortunately, this is an issue that is not resolved by time and growth, but will require surgical intervention instead.
This is discouraging, because the surgery will be fairly invasive and require 1+ week of recovery in the hospital, just when we thought we were on surgery “hiatus” for awhile. But this is a short-term setback for a long-term gain.
The end goal is still decannulation, it just may be under a different timeline than we anticipated.
We will take the next couple of weeks to regroup and see our local team of doctors for follow-up appointments to discuss plans for surgery. We are also in communication with our team of Boston docs to get their opinion on this issue and see whether we need to potentially travel up their way for this surgery.
Please know that Tucker is doing well at home, and was just as happy with his trach back in yesterday as he was with it out, which is perhaps perspective for all of us in this. We have some good friends whose son Camden has a medical history with similarities to Tucker. The tagline on their blog for their son is “joyful living in the midst of adversity.” We’ve always loved that.
And we are still celebrating how far Tucker has come and the joy that he radiates, even when difficult circumstances arise along the journey.
May 28, 2015
It’s been so long since we wrote an update on this blog, I forgot my WordPress username and password.
I will keep this update brief, that way you can skim the highlights.
- In April we took Tucker to Orlando, Florida to meet his hero Mickey Mouse (did you think I was going to say Jimmy Fallon?) and experience Sea World. It was the first family vacation we took since Tucker was born.
This trip felt like such a gift – a celebration of how far he has come in the last three years. Tucker soaked it all up. He asks to watch the iPhone video of him dancing at the Parade of Characters through Main Street in Magic Kingdom no less than ten times a day.
- Our dear friends the Blancos allowed us to join them at Sunset Beach a couple of weeks ago and Tucker got to experience the beach for the first time (a lot of firsts for our family in the last six months!) After some initial anxiety about the sand, he did great and loved it.
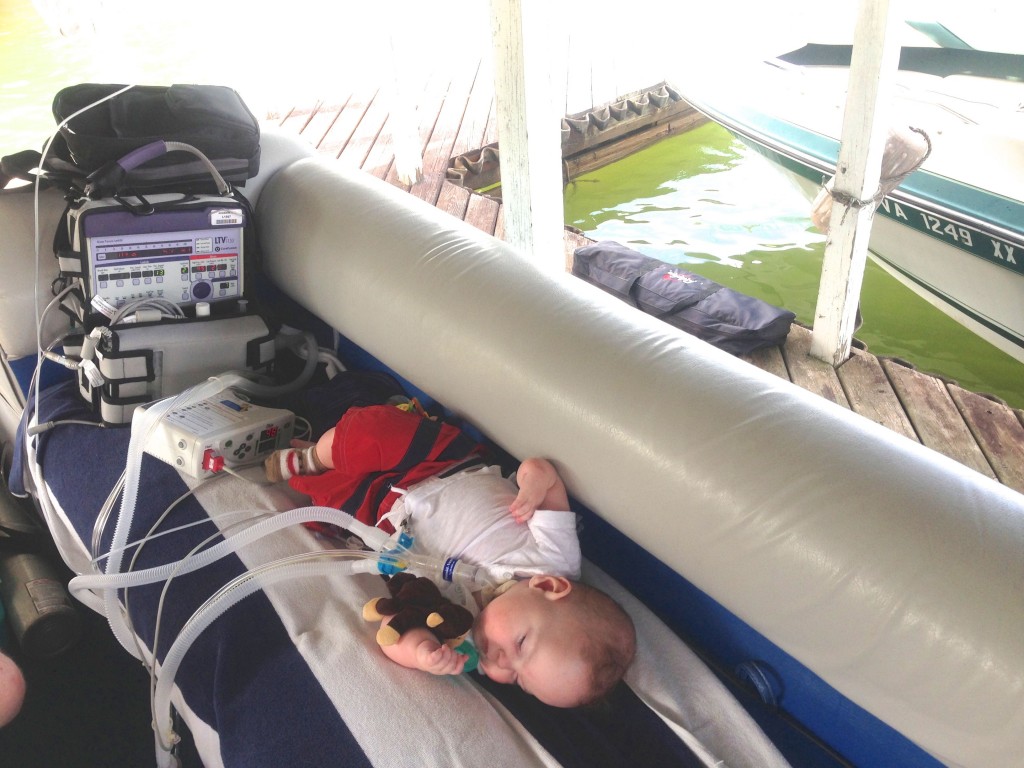
- Lake season is back. Enough said.
- June 24th, Tucker is scheduled for a bronchoscopy and decannulation (e.g. where the doctors will take his trach out permanently). The process is: his ENT will take him down to the OR, take a look down his airway using a scope, send him up to the Pediatric ICU to recover, and pull the trach out once he sleeps off some anesthesia.
They will keep him overnight and monitor his oxygen saturations and make sure he’s not working too hard to breathe. If all looks good overnight, they will send us home the next day trach-less to let the hole begin to close up.
So. many. feelings. This is a big deal. We are both excited and nervous. If you could pray for June 24th, that would be a blessing to us.
Tucker will turn 3 on July 13th. He will begin pre-school two days a week at a local church near our home this Fall. We are so excited for him!
Lots of folks have asked when our next trip to Boston is…the short answer is we don’t have any on the horizon for quite a while. Tucker is done with planned surgeries until elementary school, when we will continue to do some corrective procedures on this arm with radial aplasia.
Random highlights and facts about Tucker:
- Loves: Jimmy Fallon and the Roots, Thomas the Train, Mickey Mouse and Donald Duck, Jake and the Neverland Pirates.
Also loves burping, making you smell his feet after you take off his shoes at night, and watching videos of himself on an iPhone.
-Dislikes the Happy Birthday song (we are working on it before his 3rd birthday).
-Thinks Tommy is the most hilarious person on the planet (somebody has to!)
-Enjoys snuggling with me when he wakes up from his nap. Currently he’s napping an average of 2 out of 7 days a week so I am catching those snuggles when I can.
Operates life with wild curly hair and a joyful spirit. Pretty much sums him up.
December 2, 2014
We have been slow in posting an update since Tucker was discharged from the hospital last week, everything happened so quickly. Tucker was discharged on Wednesday afternoon. JetBlue (the only airline we will fly from now on, forever) graciously changed our return flights for the third time so that we could fly back home on Thursday morning. We got back to Richmond and got right in the car and drove to Virginia Beach to celebrate Thanksgiving with family.
We were so grateful to have Tucker released from the hospital so that we could make it home for Thanksgiving. Many of you prayed that this would happen, and we just want to say thank you. We had a quiet weekend at home this past weekend, and we’ve said it several times – there’s nothing like an extended hospital stay to make being at home as a family feel like a luxury.
We head back up to Boston in a little less than two weeks (Monday, December 15th) to have Tucker’s cast removed and his pin taken out. Fingers crossed, this will be a quick trip and Tucker will not catch any bugs on the plane or in the hospital.
We haven’t posted many pictures lately, but we are excited to share some of the family photos our sister-in-law Sarah took before we left for Boston. They were taken in Libby Hill Park in Richmond.
November 25, 2014
We are on the up and up! Tucker seems to have turned a corner and is having a great day. He’s been able to stay off CPAP through the vent all day, and we’ve been able to wean his oxygen down to his baseline level (.5 liters per minute). They will keep him again tonight. He could be discharged tomorrow, depending on whether he can successfully stay off the CPAP through the night tonight. He has enjoyed a little more freedom today walking around his room, and getting out of bed.
November 24, 2014
Tucker is about the same as he was yesterday. After the team rounded this morning, we made the decision to go ahead and rebook flights for Friday of this week, which means we will stay in Boston for Thanksgiving. We were to change our flights home for no additional charge, so we are grateful for that.
We still aren’t sure when Tucker will be discharged, and we are hopeful that he will turn a corner here soon. He is still receiving CPAP through the ventilator 24/7, so our first step is weaning him back off of the vent and getting his oxygen requirements down. The doctors hope to trial Tucker off the CPAP today and assess his breathing without the extra help from the ventilator.
In the meantime, we are suctioning some really nasty stuff out of his trach and his nose and trying to keep him comfortable. He is mostly wanting to sleep, or watch Elmo.
November 23, 2014
Well, we’ve had a bit of a rough weekend. Turns out Tucker has parainfluenza, which is basically a yucky respiratory virus, that’s extending our stay at Boston Children’s Hospital post-op. We started to wonder if something was up yesterday morning, because Tucker was still on increased oxygen support (expected for right after surgery, but not two days after), and we noticed his chest was tugging and he was really working hard to breathe. Since we were already inpatient in the PICU, the team was on top of things and ran cultures and a chest x-ray to confirm that he’s sick.
They’re saying this is a pretty slow moving bug, and since Tucker already has comprised lung function from being a preemie, it could take him a little more time to get over this. Best case scenario, we are able to be discharged on Wednesday and fly home to Richmond in time for Thanksgiving. Conservatively speaking, we could be here until the end of the week.
We are thankful that Tucker is in the absolute best care here at Children’s. We are also thankful that we were able to extend our stay at the Yawkey Family Inn in Brookline through next Saturday, November 29th. We are especially grateful for friends here in Boston who have been checking in on us and offering to host us for Thanksgiving if we are still here.
If you could pray for Tucker’s healing that would be great. A respiratory flu + a hand surgery recovery = a double whammy.
If you could pray for Tommy and I, for patience, for grace with one another, and perseverance. In general, Tucker at age 2 has been the hardest age to have him at the hospital. He feels miserable, so he is really sad, clingy, and doesn’t want us to leave. We are feeling weary for sure, and missing our sweet, smiling, joyful boy.
Lastly, if you could pray for flight logistics this week, that would be huge. We were scheduled to fly home this morning, but now that our stay has been extended, we are hoping to be able to fly home later in the week (and not get hit with a bunch of ticket upgrades and charges given the holiday).
November 20, 2014
10:00 pm.
A quick update after a very long day. Tucker’s hand surgery went well, and the surgeon was able to accomplish everything he hoped. He took a nerve from Tucker’s ring finger and transferred it to his thumb, and widened the webbing between Tucker’s thumb and his pointer finger. He did some other cool things to improve function, too – but since we are not very well versed in orthopedic surgeries, we won’t attempt to reiterate. What we do know (and pray) is that this surgery will really optimize Tucker’s function of his left hand.
His recovery has been a little tough, which is why the update was so delayed. Tucker spent about six hours waiting in the recovery area while the doctors tried to decide whether he should go to the PICU or the floor. Ultimately they decided to send Tucker to the PICU for the night so that he could be monitored under closer supervision, with a smaller nurse-to-patient ratio. Tucker is doing fine from a respiratory standpoint, and not needing any CPAP or pressure support – but he is on some increased oxygen and he’s having difficulty maintaining his sats when he starts crying or gets upset…which has been most of the afternoon.
We are hoping a good night’s sleep and getting some good pain meds on board will help Tucker recover well tonight.
November 19, 2014
We are back in Boston for what will likely be our last major surgery until grade school. Tomorrow, November 20th, Tucker is having surgery on his left thumb. Since Tucker was born with radial aplasia (meaning he is missing his right radius bone, and right thumb), his left hand is his dominant hand. Although Tucker has all five fingers on his left hand, we noticed from an early stage that his left thumb is weak and malposed. When we came through Boston in September, Tucker’s orthopedic surgeon recommended strengthening Tucker’s “hypoplastic left thumb” so that Tucker can have optimal function of that hand. If the surgery goes as planned, it will give Tucker a much better pincher grasp, which will be especially important for fine motor skill development and learning to write in elementary school.
Tomorrow’s surgery should last 1.5-2 hours and he is on the schedule to go into the OR at 11:30 am. We are anticipating one – two nights in the hospital post-op, depending on how Tucker recovers and his respiratory status.
We will update again tomorrow evening with details of the day, and Tucker’s recovery.
September 9, 2014
Last week was a week of “firsts.” First haircut, first dentist appointment. (You can guess which of those went better)….
We head to New England at the end of next week for my dear friend Maria’s wedding. We will spend a couple days in Boston at the end of the trip for some outpatient follow-up appointments. Can’t wait to see friends and our home away from home.
August 5, 2014
I had every intention of posting photos after Tucker’s birthday party a few weeks ago. And then suddenly, it was August and well, here we are.
I have to admit, 2 snuck up on me. We were ready for 1 – waiting for it, surviving up until we hit it. And when he turned 1, I mostly experienced intense relief and gratitude. We made it, and we celebrated accordingly.
While the gratitude remains, 2 feels different. For me, 2 was weirdly bittersweet because for whatever reason, it hit me that he is looking, acting, and becoming more and more of a kid. The long messy hair, the funny toddler words, the innate desire for independence…but the sweetness and the funny little personality mixed in between. I wish time could stand still.
July 13, 2014
Happy 2nd Birthday to our joyful, resilient boy. It is a privilege being your parents.
Tucker Turns 2 from Tommy Sibiga on Vimeo.
July 1, 2014
Tucker turns 2 this month. I feel like we were just planning his first birthday party, but in reality so much has changed from 1 to 2. We will post a recap video of his 2nd year on his actual birthday (July 13th). Until then, here are a few photos of life lately:
June 17, 2014
So a lot has happened since our last update.
We took a trip to Boston (Tucker’s first commercial flight), which went great. Tucker got his cast off, had a wicked cast rash afterwards, then got his esophagus looked at, spent an unnecessary night in the PICU (to recover from his esophagram).
(Disclaimer: Tucker’s skin does not currently look like that).
Then we discharged from the ICU, took Tucker on a quick tour of Fenway and Newbury Street, and got on a plane and flew home.
We managed to squeeze in some time with our buddies the Conleys and a few nurse and doctor friends in the 48 hours we were there.
Tucker saw his local pulmonologist here in Richmond who confirmed what we had been suspecting this spring – Tucker will keep his trach this summer and through another winter. Essentially, Tucker still needs too much oxygen right now to help him breath before his doctor will consider taking the trach out for good .
Likely, the trach will come out next spring / summer of 2015. An ongoing prayer request is that Tucker would be able to wean fully off of the oxygen.
Otherwise, we have been enjoying the summer and the opportunity to spend more time outside.
Here a few photos of life lately:
May 12, 2014
We head back to Boston a week from today (Monday, May 19th) to take Tucker’s cast off and check in with his neurosurgeon as a follow-up to his tethered spinal cord release. Tucker also will have an EGD done on Tuesday to check his esophagus and make sure the connection site looks good and healthy. We will fly back Wednesday, May 21st. It will be a quick trip!
We are flying commercial this time, and we are fortunate that our flight is direct (a little over one hour from Richmond to Boston). I am working on a bunch of logistics to get Tucker oxygen on board the flight, get medical supplies and equipment organized to go through security, etc. Prayers for smooth logistics leading up to our trip next week would be huge!
Here are a few photos of life lately:
April 22, 2014
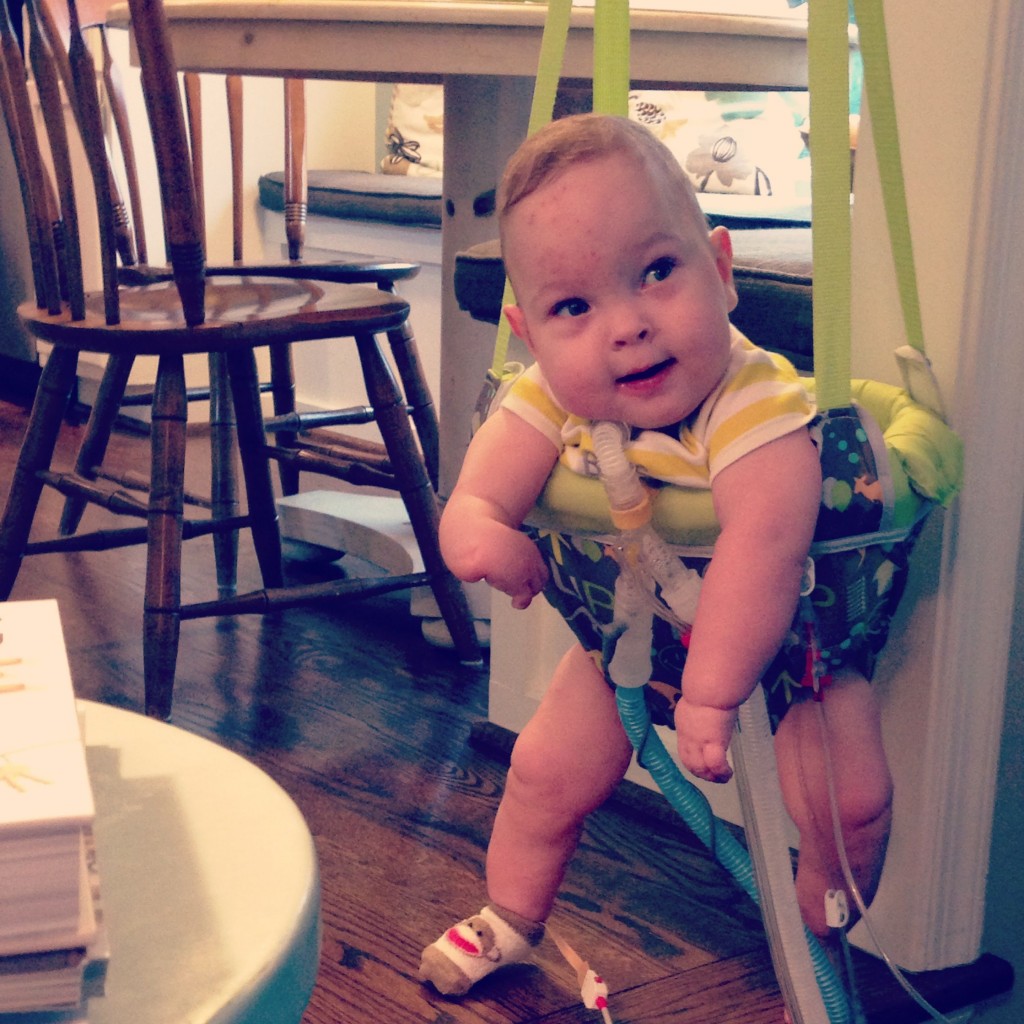
One year in with the trach.
(We passed the anniversary of Tucker’s trach surgery last week).
I think these two photos capture the stark contrast between life before and after Tucker’s trach.
When we trached him, it was like we met Tucker for the first time.
After eight months of his little body focusing all of its energy on healing and breathing, the trach surgery gave him the opportunity to thrive. And to come home.
That season of preparation to leave the ICU feels especially poignant for me right now, because of the season change, because we are approaching the one year anniversary of bringing him home.
And because I’ve been in communication with a couple of other moms, new to the trach journey like we were this time last year. The mixed feelings of anticipation, anxiety, intimidation are so familiar. Figuring out how to hire and schedule nurses, practicing trach changes in the hospital, learning the equipment set-up and how to essentially simulate a step-down unit in your own home. It is daunting.
(Those of you who were that experienced trach mom for me a year ago, thank you. You know who you are. You are so loved).
It is the start of a journey that will require the bravest, smartest, most selfless fibers of your being. Qualities you didn’t know that you had, or qualities that had been there all along, and never had the opportunity to emerge until now.
You will see these qualities within yourself. You will see them in your spouse. And you will be reminded of the gift that you have in each other. That you were uniquely created to live this life, to raise this specific child, together. And that will add a depth and a maturation to your marriage that is immensely rich.
Easter morning this past Sunday, Tommy and I were standing in the kitchen; Tommy was making coffee, while I leaned against the kitchen counter in my pajamas, priming Tucker’s feeding pump.
He looked over at me as he was pouring coffee into his mug, and with a smirk, he cut his eyes at me and said, “Want to guess what you did last night in your sleep?”
I shook my head and brushed sleep out of my eyes. I smiled an embarrassed smile. “No, I don’t need to.” I said. I already knew.
“I tried to change ‘your‘ trach, didn’t I?”
Tommy laughed at me and nodded. I remembered the night before, when I dreamt Tommy was Tucker and I kept feeling his neck, prodding my thumb into his sternum, frantically making sure that “his trach was in.” Until I woke up and realized I was dreaming, and that the “naked neck” I was feeling was Tommy’s and not Tucker’s.
“You do that kind of stuff a lot when you sleep, you know.”
He’s right, I do.
Although time has faded many of the memories surrounding the first night we brought Tucker home, you never really forget what it’s like to code your child at home.
It still lives somewhere, deep in your subconscious.
I remember the discordant sound of ventilator alarms, our suction machine, and Tucker’s pulse oximeter ringing off in the middle of the night….Not being savvy enough at that point to silence them in unison so that they didn’t add to our mounting anxiety level.
I remember frantically bagging Tucker’s trach over the side of his crib, alternating giving breaths while Tommy did chest compressions on his little chest. And I remember watching the numbers on his pulse oximeter slowly crawl back up as his oxygen saturations and his heart rate stabilized, only to dip down and come back up again, the entire ambulance ride to MCV.
A year later, we are all three better for that night. As as awful as it was. (And we are so very fortunate no damaged was sustained).
We are all three of us, better for the last year really…and all that came with it.
I am continually humbled by what we are learning, as the stewards of this child. That out of most difficult and challenging circumstances, can arise a strength and a joy you never knew.
April 7, 2014
We are home! After what was the quickest hospital admission we’ve ever had.
Tucker handled the recovery from his wrist centralization and tethered cord release like a champ.
Boston Children’s Hospital discharged Tucker on Saturday afternoon. We had dinner in Boston with our wonderful friends the Conleys, and then we got on the road and drove back to Richmond Saturday night/morning.
Tucker will have his arm in a cast/sling for the next four weeks until we return to Boston for some outpatient appointments to have the cast and the pin in his wrist removed.
We are thankful to be home so quickly, and especially thankful Tucker handled these surgeries so well! Here’s to being bigger, healthier, and stronger, with every trip to the OR.
Tucker also came home with a speaking valve that allows him to make noise through his trach. He loves hearing himself talk!
Tucker Talking with Speaking Valve
April 4 – 8:00 am
Tucker had a good night post-operatively. They were able to manage his pain overnight with Tylenol only – we will continue to watch him today and see if he will need morphine intermittently.
Tucker came back from the OR on the ventilator, but they were able take him back off the vent last night as he started to wake up and the anesthesia left his system.
He is acting more like himself today, but we definitely have not gotten any smiles or silly faces. We can’t blame him. He has an IV in one hand with a board, a cast on the other arm, and he has to lay flat in bed all day while his surgical site at the base of his spine heals.
Watching him sign to “stand up” with his big bulky cast is about the cutest and most pitiful thing we’ve seen.
Pray for patience for him and for us today! Tomorrow (Saturday morning) he will be allowed to sit up again and start resuming normal activity.
I foresee a long day of movies on the I-pad ahead.
April 3 – 5:00 pm. Back from the OR.
Tucker is back from the OR and sleeping. His arm surgery went well. Dr. Waters was able to straighten his hand onto his wrist. He has a big green cast on his right arm that he will need to wear for the next month, until we return to Boston in May for an outpatient visit to have the cast removed. He also has a pin in his wrist that is holding everything in place. The pin also will come out in May when his cast is removed.
Dr. Waters did not make any surgical changes to his ulna bone in his forearm. Tucker’s ulna is slightly bowed due to his anatomy. Dr. Waters said this will often self-correct as it grows, with his hand now straightened. If it does not self-correct, we will reassess surgery on his ulna bone down the road in combination with a thumb pollicization.
Tucker did have a transient blue spell in the OR, which was a little disconcerting for us to hear about. Apparently he turned blue and dropped his sats very quickly. The doctor said it was very short and no damage was sustained. They gave him a dose of epinephrine which brought him out of it.
Typically when Tucker has spells like this at home, it is related to his airway and he is not getting good air exhange. We noticed when he came up from the OR that his secretions were very thick and difficult to suction. We went ahead and did a trach change at the bedside and bagged in some saline to help loosen the mucus from the bottom of his trach.
We aren’t sure whether a plug was the source of the brief blue spell in the OR, but they will continue to watch him closely while he recovers from surgery.
Tucker’s next 36 hours will likely frustrate him. He has to lie flat on his back (or stomach) to prevent any spinal fluid from leaking out of his surgical site on his back. His cast also goes from his hand to his arm-pit.
So, as he wakes up and realizes he can’t sit up or stand up, and he has a clunky cast on his arm, we suspect he will be an unhappy guy.
Please pray for patience, healing, and grace.
April 3, 2014 – 1:55 pm
Dr. Proctor finished Tucker’s release of his tethered spinal cord a little after 1 pm. He said the fatty filum tissue that he separated away was actually thicker and tighter than we anticipated from Tuckers MRI in October. Will be interesting to see how that affects walking/crawling.
Dr. Waters just started on Tucker’s arm.
April 3, 2014 – 12:00 pm
Tucker went into the OR around 10:15 am.
His admission this morning went smoothly. They allowed Ellie to gown up and carry Tucker into the OR so that she could hold him while they put him under. (Yet another reason we love the level of family-centered, quality care at Boston Children’s Hospital).
We anticipate Tucker will be in the OR for about six hours, since they are doing more than one surgery.
His tethered spinal cord surgery will be first and take about 45 minutes. They orthopedic surgeon will operate afterwards.
A nurse liason updates us every 90 minutes, so we will update the blog as we receive updates.
March 24, 2014
Tucker is doing better as the “chest cold that never ends” seems to actually be coming to an end.
We put him on antibiotic towards the end of last week. Whether the antibiotic was the game-changer or it was a slow-moving virus that just needed to run its course, its nice to see Tucker’s energy level return to normal.
He is still on some increased oxygen support from his “normal,” but I am hoping to wean his oxygen back down over the next few days in time for our big trip to Boston next Tuesday.
Ed We will leave Tuesday night, April 1st and drive through the night. We’ll leave between 8-9 pm and arrive in Boston between 6-7 am.
We will admit Tucker at 11 am that Wednesday morning, April 2nd.
Both surgeries are scheduled (under one anesthesia) for Thursday, April 3rd.
We are continuing to work on logistics for our stay in Boston. We anticipate being there about a week. Looking forward to seeing old friends and faces (and hoping we bring some warm weather with us) as we head north.
March 16, 2014
You are only as good as your child.
The last eight days, Tucker has been all over the place. So, so have we.
Wednesday he feels great, Wednesday night he runs a fever. Friday night he makes the night nurse work her tail off, suctioning. Saturday he’s great again – we go to Home Depot. Then he starts coughing yellow crap out of his trach.
Since last Sunday, Tucker has been fighting some kind of weird respiratory virus that is only in his lungs. Awesome, right?
I think I have suctioned more junk out of Tucker’s trach in the last week than I did the whole month prior.
I am beginning to wonder if it’s Mother Nature’s final kick in my butt at the tail end of the winter that almost killed all mothers who have young children. That’s what I am calling the Winter of 2014, by the way. The winter that almost killed all the mothers of young children.
I took Tuck in to see his pediatrician earlier in the week, and then we touched base again over the phone yesterday. (Because our pediatrician is amazing and lets me harass her on her personal cell on the weekends). She feels like this is a virus, and we agreed that we want to maintain Tucker at home as long as his vitals remain stable and he’s not spiking a temp.
Tucker’s vitals have remained stable (with some increased oxygen support and nebulizer treatments). So, we are muddling through. I feel somewhat like I’ve been living under a rock the last week, and will be thankful when he is through whatever this is.
If you wouldn’t mind praying for him – that he would get over this bug in plenty of time for our trip to Boston. And for us, that we would have the confidence and fortitude to manage this one at home. Especially with the impending snow storm. Woof!
March 6, 2014
Surgery is a “go” on April 3rd in Boston. Both of ‘em. (Wrist centralization and spinal cord de-tethering).
We will likely drive through the night again like we did in October. It’s about ten hours from Richmond to Boston and worth the all-nighter to have a sleeping toddler vs. a whining toddler in the back seat.
We will do some pre-op appointments on Wednesday, April 2nd then Tucker will go in for surgery on Thursday, April 3rd. Anticipated stay in Boston including recovery is about a week.
A few folks have asked why we are headed back to Boston for surgeries that are not “esophagus-related.” Here’s why….
1) We love Boston Children’s Hospital and think the quality of care and expertise they offer (especially related to complex medical children like Tucker) is the best of the best. They are hands down, part of the reason why Tucker is thriving as much as he is.
2) Tucker’s particular arm birth defect, called “radial aplasia” is rare enough that local orthopedic surgeons don’t feel comfortable operating on it here in Richmond.
3) Tucker’s tethered spinal cord could be detethered here in Richmond (we consulted with a local pediatric neurosurgeon who we liked very much).
But…since both surgeries need to be done within the next 6 months, we want to combine anesthesia, pain meds, and hospital stays into one. Easier on Tucker and on us.
Another question folks have been asking frequently is when Tucker will get his trach out for good.
Likely, this summer or next spring. Here’s what is currently preventing Tucker from getting his trach out:
- Oxygen need. Basically Tucker needs to get off continuous oxygen and be able to maintain his oxygen saturations successfully. We are getting closer but it is a slow process. Time and growth heal chronic lung disease related to prematurity. So we are growing and waiting. And praying.
- Big surgeries still on the horizon. Perk of having a trach? Tucker does not have to be intubated right now for surgery. i.e. He doesn’t need a breathing tube down his throat because he essentially already has one in the form of his trach. When Tucker goes into the OR for surgery, they essentially just plug him into a ventilator and he’s good to go.
February 16, 2014
We have a tentative surgery date for our next trip to Boston – April 3rd. This trip to Boston is not esophagus-related (although we may try to squeeze in a visit with the Esophageal Atresia team because, why not?).
The April 3rd OR date will include two surgeries under one anesthesia:
1) De-tethering of Tucker’s Spinal Cord (done by a pediatric neurosurgeon)
2) Wrist Centralization (corrective hand surgery done by an orthopedic surgeon)
We anticipate this trip will likely be 1-2 weeks depending upon Tucker’s recovery, etc.
More details on that trip as we get them…
Tucker also had a routine bronchoscopy this past Wednesday, February 12, the results of which could explain part or all of the lethargic episodes he was having the week before. (Tucker had two more episodes similar to the one last Monday where I had to do an emergency trach change).
We suspected Tucker had something in his airway below his tracheostomy tube that was prevent Tucker from getting good air exchange.
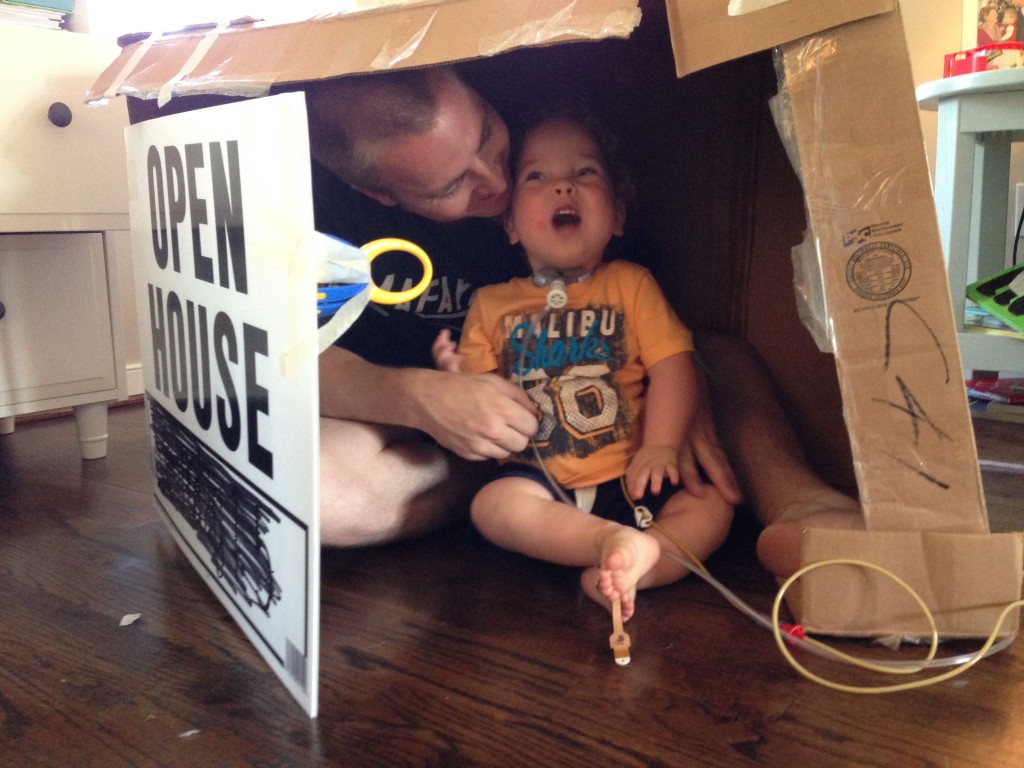
Turns out we were right and Tucker had a big granuloma in his airway…
The best way we can describe a granuloma is like a blister on the inside of Tucker’s airway. It’s essentially the body reacting to a foreign object that is not supposed to be there. As long as Tucker has the trach, he runs the risk of developing interior granulomas.
Fortunately, we have a wonderful ENT doctor who follows Tucker here locally and she does a routine scope every 6 months to make sure these granulomas get taken care of.
She removed the granuloma above during his bronch and Tucker has not had any more lethargic episodes (AND we’ve been able to reduce his oxygen level by almost 50%). Down from 1.5 liters continuously to 3/4 liter continuously.
February 4, 2014
Tucker kicked off the week by needing an emergency trach change yesterday morning.
Thankfully, I was at home and I could hear our night nurse downstairs talking to him and asking why he had gotten so sleepy all of the sudden. I came downstairs, took one look at Tucker’s face and I knew he wasn’t sleepy, his trach tube was occluded and if we didn’t act quickly his vitals were going to tank.
I grabbed some lubricant and a spare trach out of our supply closet and our nurse layed him on the floor, tilted his head back, pulled his trach out, and I put the new one in.
No drop in sats or his heart rate, but he went from lethargic and unresponsive to pissed and alert as soon as the new trach was in. I have done three emergency trach changes, and it happens this way every time.
Tucker coughed up about a half teaspoon of blood afterwards, which warranted me calling the doctor to see if they wanted us to come in. His pediatrician was okay with it, so long as the blood stopped, which it did. Said I probably just irritated Tucker’s airway a little bit with the rapid trach change.
I’m not sure in what world having your 18 month-old cough up blood is normal, but I guess in ours it is.
So the situation stabilized and our nurse left. I took Tucker upstairs and put him down for his nap.
And then I went into our master bathroom and I dry-heaved…
We’ve been home for eight months, and that look on his face still makes my adrenaline surge.
The glass-eyed, doesn’t recognize my voice, doesn’t respond “look” that is my warning to put on my big-girl pants or Tucker would be blue, and we would be taking a $2,000 ambulance ride down to VCU.
Life is fragile. I was humbly reminded of that yesterday. Those are the moments where Jesus is most real and present to me, knowing what might have taken place otherwise.
We are working on scheduled an arm surgery and a spinal cord surgery for this spring, likely March in Boston. More details to follow. Otherwise, we are great!
January 15, 2014
This is Tucker eating yogurt.
This is our son, who was born 15 weeks premature and with an incomplete esophagus, who has been completely tube-fed for the first 18 months of his life….who is eating.
Small bites and with slow progress, but Tucker is eating. Guacamole. Yogurt. Rice cereal with fruit.
I realize this may seem inconsequential to some, but in our family, we have learned to take nothing for granted.
This is a lot of hard work and learning oral motor skills that he missed out on as an infant.
I wish someone could have showed me this photo last January. When Tucker was in Boston under medical paralysis as they grew the two ends of his esophagus together, and I just prayed fervently for all of it to be over.
I probably would have wept.
Thank you for praying for our son to get here.
He is thriving.
We are so proud of the progress he continues to make. We are grateful for this season of abundant joy and growth in Tucker’s life. God is good and faithful. In every season.
December 27, 2013
Christmas at Home.
December 5, 2013
This update should really just say, “Look, ma – no ventilator!”
As of about two weeks ago, Tucker is only on the vent while sleeping.
Tucker is doing amazing and we have so much more mobility without the ventilator. I jokingly refer to Tucker’s vent as his “ball and chain” so we are feeling free, free, free!
I took Tucker to the park yesterday on just an oxygen tank and it was GLORIOUS.
After Tucker’s “swallow” study on November 19th, we also got the thumbs up to start introducing oral feedings. (Up until this point, Tucker remained tube-fed while we waited for him to heal from his Nissen Fundoplication surgery).
Getting Tucker to the point where he eats by mouth will be a slow and delicate process. Since Tucker is eating so late, we will skip the bottle entirely.
Right now, we are introducing a spoon to Tucker. No food yet – just the spoon. Tucker has to allow us to put a spoon in his mouth without pushing it away before we can put food on that spoon. We do not want Tucker to develop an oral aversion or be afraid to eat since all of this is a very new experience for him.
So for now….we are simply putting a spoon in his mouth and hoping he doesn’t throw it back at us. But hey, it’s a start! A prayer request would be getting some food on that spoon.
Here are a few recent family photos that our talented sister-in-law Sarah Lynn took in November. If you want to see more of her work, you can check out her Facebook page here.
A few people have asked about our anchor tattoos. We got them on our most recent trip to Boston, the same day Tucker had his Nissen Fundoplication surgery. The anchors represent a significant scripture verse for our family (Hebrews 6:19) and the hope that we have, anchored in Christ.
Sunday, November 17, 2013
These are the two greatest people you will ever meet.
That’s my dad on the left and my mom on the right.
It also happens to be their birthdays today and tomorrow.
Tonight, we celebrated “Saunders Family Birthday Week” at my brother and sister-in-law’s house. As we sat around the dinner table with Tucker in his high chair next to us, I remembered back to last year. We spent most of “birthday week” in the NICU next to Tucker’s hospital crib. He was still sick and small and fragile and probably on precautions for some type of respiratory infection.
I thought about how far we have all come. I thought about what it means to be a parent. Who I am as a parent.
And I looked at my dad holding my big, healthy, smiling boy – who was sitting on his lap and grabbing his beard and glasses, and I felt the feeling that permeates my thoughts….every single day. I am so fortunate.
They are the best parents.
And I am so thankful for them. I wouldn’t be half the mother, half the wife, half the person I am today if God had not gifted me with the two of them.
Sometimes my heart hurts for them – for the first year they’ve had as new grandparents. There are so many rights of passage and first grandchild moments that I worry they were deprived of. Just as Tommy and I are in the season where most of our friends are young parents having babies, they are in the season where most of their friends are young grandparents having grandbabies.
I struggle knowing that their journey has looked different than their friends, probably in the same way that they struggle knowing that our journey has looked different than our friends.
So many of the teachable “grandparent-to-new-parent” moments have felt lost on our family.
A NICU nurse taught me how to change my son’s diaper. Change his g-tube dressing. Suction out his nose. Suction a trach tube. Change his trach. Change his trach ties. Hook up a feeding pump bag. Give subcutaneous blood thinner injections. Perform CPR.
But you know what my mom taught me?
Grace.
In the midst of heartache. In the midst of fear and anxiety.
My mom taught me Grace.
Grace and Trust.
My whole life, she’s taught me that. To take each day, one day at a time. To not be a victim of my circumstances but to have faith that the journey God set me upon is purposeful and for his glory. She taught me that God doesn’t guarantee “easy,” but we can trust in His Goodness. My mom is the voice in my head that always whispers, trust, when I want to go running and screaming in the opposite direction.
She is my anchor, my earliest teacher of faith, the woman who sang the same hymns to my younger brother and I that I now sing with Tucker when it’s just the two of us, alone in the house.
And my dad.
I have this memory of my dad teaching us how to water-ski at our family’s lake house on Buggs Island Lake. This memory has been at the forefront of my mind the last year with Tucker. My dad started us on water skis really young.
That was pretty much his style with anything that required some measure of risk and bravery for a little kid.
I have this image of him at the steering wheel of the ski boat, idling the motor and wearing this old t-shirt that said “Go Hard or Go Home.” I would be 20 feet behind him in the water holding onto a tow-roap with my skinny legs knocking my water skis together, while I shivered in my Little Mermaid life jacket. And my dad would crank his head around, with his two-day scruff and “lake” hair, and yell back to me, “Ya ready?”
And I knew, for better or worse, I needed to yell back “Hit it!” (which meant crank the motor) at which point I would either slowly make it up over top of the wake or I would suck down a stomach full of lake water.
I spent a good amount of time the summer I was 6 sucking down lake water and getting dragged, face-first, while I clung to the handle at the end of the tow rope.
Regardless of whether I got up, when I finally tired out my dad would pull me back into the boat and tell me “good job.”
And I eventually, I did get up. And I learned to ski more aggressively, with confidence, and with skill.
But I had to choke down a lot of lake water first to get there, and for whatever reason that is the metaphor that comes to mind for me when I think about my first year as a mom to Tucker.
I think about my dad.
I think about all of the deliberate opportunities he gave me throughout my childhood to choose tenacity instead of caution.
He is the voice in my head that reminds me that I am strong, resilient, and that I am capable of much more than I ever thought.
There is no manual, no book for raising a child like Tucker. There is no way that my parents could have taught me all of the skills and nursing that would be required to keep Tucker well.
But you know what, they didn’t really need to….
They taught me, from an early age, much greater foundational truths about life and faith and parenthood.
To walk in grace, to be brave, to love deeply….and to know that my story and my child’s story are simply part of a greater story.
Happy Birthday, Mom and Dad. You are so very loved.
Friday, November 1. 2013
November. I can’t believe we are here. It’s been a big week for Tucker with lots of changes and medical milestones, but somehow that seems overshadowed by the fact that we took him trick-or-treating last night.
That may sound trivial, but we spent five holidays in the hospital last year, the first of which was Halloween. Yesterday, I looked back at the picture of Tucker last Halloween in the NICU at Henrico Doctors.
Halloween 2012….
And when we put him in his sock monkey costume yesterday and loaded him into his new red wagon to go trick-or-treating with some dear friends, I felt a lump rise in my throat.
Halloween 2013
Life doesn’t necessarily look like we thought it would a year ago, but man we are living. And we are blessed with a child who despite many hurdles and physical challenges, exudes JOY.
Not because Tommy and I are faithful people all of the time, but because Tucker is God’s faithfulness made manifest.
So mostly this week, I am just overwhelmed with gratefulness. For where we are. For how far Tucker has come. For opportunities to dress up like a life size sock monkey and be a little boy with his buddies.
Some details on the changes that were made this week:
- We went to general surgery on Monday and took out Tucker’s G-J tube and replaced it with a G-tube. Before Tucker’s Nissen Fundoplication, he was fed “jejunally” to his lower intestines on a continuous rate. This means he was hooked up to a feeding pump/milk bag 24 hours a day.
- With Tucker starting G-tube feedings again, we are able to give him “bolus” feeds now so that he gets food intermittently throughout the day (on more of typical eating schedule) and he’s not hooked up to a feeding pump all the time.
- Tucker also saw a dietician who wrote up a new feeding schedule and gave me the green light to start adding blenderized baby cereal, fruit, and veggies to Tucker’s formula.
- Tucker is not okay to start eating by mouth until six weeks post-Nissen surgery. (We are four weeks post-op).
- Once Tucker gets cleared to start eating, his biggest challenge will be learning how to swallow without aspirating his food into his lungs.
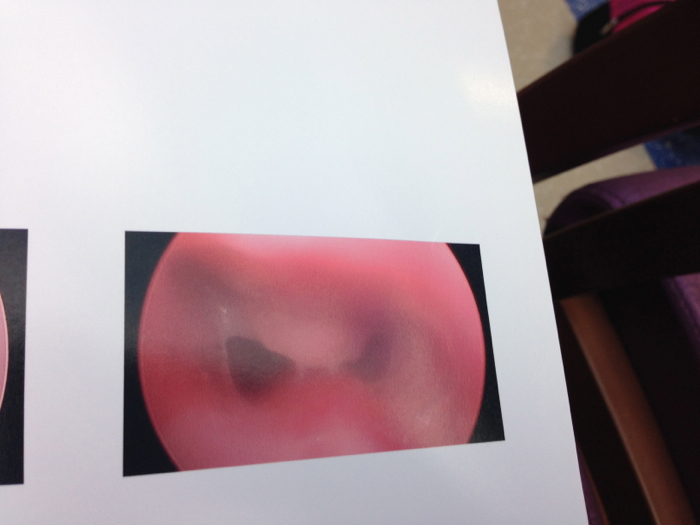
- Tucker’s pulmonologist gave him the go-ahead to start trach collar trials yesterday. This too, will be a slow process of weaning Tucker off of the ventilator and simply onto just a trach collar with some oxygen.
- Because we don’t want Tucker to wear out too quickly, we won’t ditch the ventilator right away.
- Right now, he’s doing two hours a day off of the ventilator and we will continue to increase that as Tucker’s lungs tolerate it. The goal is to get Tucker on a trach collar during the day and on the ventilator at night.
- We will likely keep Tucker on the ventilator while he sleeps at night, through the winter.
- Here’s what the trach collar looks like:
- We met with the pediatric neurosurgeon today out of MCV, Dr. Tye. He reviewed the MRI images Boston took of Tucker’s spine and agreed that Tucker has a tethered cord. It’s low and “borderline” but Dr. Tye said it does need to be addressed.
- The good news is that Dr. Tye said it’s NOT a surgery he wants to do before the end of December. His biggest recommendation was to be home for the holidays, let Tucker recover from his Nissen Fundoplication.
- He wants us to see him again between January and March to start making plans for a tethered cord surgery in the spring or summer of 2014.
So we are staying home for the holidays, y’all….
Sunday, October 27, 2013
Tucker had a cold (again) this week, as evidenced by the sick snot bubble below. Fortunately this cold stayed “north” in his sinuses like the last one. Tucker powered through it without any increase in oxygen or respiratory support from the ventilator.
This week will be an extra busy one.
Here’s a week in the life of Tucker. Poor dude has an appointment every day with some kind of sub-specialist. Great planning, Ellie. Sigh.
- Monday – Local GI Surgeon Group to Check out G-tube Site
- Tuesday – GI Nurse Practioner to Discuss Diet and Feeding Schedule
- Wednesday – Occupational Therapy
- Thursday – Pulmonary Clinic. Maybe start trach collar trials?!
- Friday – Local Pediatric Neurosurgeon Consult to Discuss Tethered Cord Surgery
If you could be praying for Thursday and Friday’s appointments, that would be wonderful. They are both big appointments for different reasons.
Sunday, October 20, 2013
This update comes a few days late, but we made it back to Richmond late Thursday night. It took us about 11 hours to drive from Boston to Richmond and Tucker did great. We stopped every 2-3 hours for breaks/snacks and only hit traffic in New York. I feel like you can’t ask for much better than that.
The best part about coming home was seeing Tucker react to being back in his nursery. He woke up when we took him out of his car seat. We put him in his crib a little before midnight. He started laughing and clapping, and patting his crib bumpers. His night nurse told us the next morning that every time she checked on him Thursday night he was smiling in his sleep.
That boy knew he was home!
As we were walking out the door of Boston Children’s Hospital (literally with stroller loaded and discharge papers in hand), the attending told us that Tucker has a tethered spinal cord, as confirmed by the MRI on Wednesday.
The fact that Tucker has a tethered cord did not surprise us so much as the neurosurgeon telling us he wants it fixed within the next two months, preferably November. We really hope to be home for the holidays this year, so we are trying to take this news in stride. We need to decide when to have the surgery and where to have it.
We could go back to Boston next month, which would mean another long road trip with a “vented” baby. We are also going to check into having the “untethering” done here in Richmond with a local neurosurgeon out of MCV. If you could pray for wisdom and discernment for us, that would be great. We will likely need to make a decision quickly and start planning for this tethered cord surgery within the next week.
In the meantime, we enjoyed some normalcy and family time at Ashland Berry Farm this morning. Tucker took his first official trip to the pumpkin patch. Since Tucker was still in the NICU last October, trips to the pumpkin patch weren’t even a possibility.
We are so happy and so blessed.
Wednesday, October 16, 2013
Tucker’s week of diagnostic testing is almost complete:
Echocardiagram on Monday– no visible pulmonary hypertension.Esophagram on Tuesday– Tucker’s esophagus and stomach looked great! The Nissen is still a little tight, but Dr. Jennings felt it looked appropriate and that it will loosen over the next four weeks as the swelling around the wrap continues to go down. The big news is that Tucker did not reflux at all and he took the contrast by mouth. For a non-eater, that’s pretty good!MRI today (Wednesday) at 3:30 pm- to check for a tethered cord, a common finding in VACTERL kids. If Tucker does have a tethered cord, we will have surgery to correct it in the spring of 2014. The best news we could get today would be that Tucker doesn’t have a tethered cord = one less surgery.Consult with Orthopedic Surgeon about Tucker’s radial aplasia (arm) – today. Currently having x-rays taken. Corrective arm surgery will likely take place spring of 2014.
The plan is to let Tucker sleep off the anesthia from his MRI this afternoon and discharge tomorrow (Thursday) sometime in the late morning or early afternoon.
We will be driving home to Richmond tomorrow (about 10 hours) so if you could pray for a smooth, safe drive with no traffic that would be great!
Here are a few photos from Monday and Tuesday….
Saturday, October 12, 2013 – 11:00 am
What a difference 36 hours can make!
Tucker is doing really well. It’s so nice to see him acting like himself again. He is back up to full formula feeds, off of oxycodin (and only on Tylenol as needed), and looking much better from a respiratory standpoint.
Although he is still on pressure support on the ventilator, we are fine with this. He came home on pressure support, and we can always wean him back to CPAP (his pre-op settings) at home. We want to keep him stable and breathing comfortably so that we can work towards discharge.
We are discussing discharge plans for next week but a few things have to happen first:
- Echocardiagram – this is a routine echo to check on Tucker’s heart and make sure he hasn’t developed any pulmonary hypertension.
- MRI of Tucker’s spine – to check for a tethered spinal cord, a common finding in kids with VACTERL. (If Tucker does have a tethered spinal cord, we will have it surgically corrected this spring).
- Esophgram – to check Tucker’s esophagus and stomach post-op.
One unfortunate side affect of the femoral artery injury last week is that Tucker will have to come home on blood thinner injections. This means Tommy or I or his nurse will have to give him injections 2x a day for about six weeks. We will re-image the artery back in Richmond to make that the area of narrowed blood flow resolves. We are praying it resolves sooner than six weeks.
Thursday, October 10, 2013 – 5:00 pm
A quick update…Tucker is doing okay. I’d give him a 6/10.
We’ve had a frustrating day in regards to some medication confusion, and some back and forth changes to ventilator settings but things seem to be headed in the right direction.
Tucker is back on pressure support (higher ventilator support).
He is also now on droplet precautions because his care team wanted to culture the mucus from his trach for infections. I feel like this happens every time we are in the ICU and while we appreciate preventative care, I am weary of the tendency to “over-treat” for infection. This seems to be a common theme among children’s hospitals.
Dang babies! If they could just talk and say, “Hey, I’m not sick! Thanks!”
There continues to be concern about Tucker’s leg where the femoral artery was injured last Friday in the OR. The concern is largely out of whether diminished blood flow to that artery will affect leg growth down the road….(insert freaked out parent faces here).
Fortunately, they have kept Tucker on heparin (blood thinner) which will be transitioned to Lovenox (blood thinner injections) that we will have to give him at home. We don’t know how long yet Tucker will need to Lovenox injections. It depends on how quickly his body heals that artery and normal blood flow returns.
As you can imagine, this has been a really frustrating and trying complication of Tucker’s surgery last week. If we need to intervene surgically and dilate the artery, we can – but we are pretty upset that this happened in the first place.
We are also discussing the possibility of discharging Tucker locally to our church apartment in Newton. If Tucker’s team is on board, the discharge will take place at the beginning of the week. We would keep Tucker outpatient with us in Newton until his two follow-up procedures next Friday to assess reflux.
Wednesday, October 9, 2013 – 11:00 am
All in all, we’ve had a good 48 hours since our last update. Tucker is back on his normal ventilator support – CPAP of 5 (and tolerating it beautifully).
We switched Tucker’s pain management from morphine around the clock to oxycodin and tylenol as needed.
Tucker seems much more comfortable, alert, and happy since that change. I took his trach cuff down yesterday morning for a bit and he immediately started singing. Nice to see our little turkey returning back to us.
Some not so great news is that Tucker has an insult to an artery in his leg where the surgeons tried to place a central IV line in the OR last Friday. This is not (new) news, but his foot/leg continue to remain cool to touch and pale in color so the attending decided to have an ultrasound done to rule out a blood clot.
Although Tucker does not have a blood clot in his leg, he does have an area of narrowing in that artery where blood flow is clearly diminished on ultrasound. The PICU has him on heparin and Tucker has been sporting some new Patriots socks to keep circulation moving to his feet.
Hopefully, this is an issue that will self-resolve before we are discharged. Worst case scenario is that the artery will need surgical intervention. Best case scenario is Tucker’s body heals the site itself and he comes off the heparin soon.
Now that we are on the road to recovery, I asked Tucker’s team about discharge plans. They want to do a repeat espohagram and gastric emptying study two weeks post-op, which puts those procedures on Friday, October 18th.
Since it’s looking like we will be inpatient a bit longer than anticipated, we may ask about trach collar trials (taking Tucker off the ventilator)….which is something we planned to do after we returned to Richmond.
Monday, October 7, 2013 – 3:00 pm
Not much has changed since yesterday’s update. I wish I could say Tucker has turned a corner.
Maybe I have a case of the Mondays combined with the fact that I dropped Tommy at Logan this morning for his flight back to Richmond.
Tucker’s PICU team decided to put him back on pressure support (10/5) this morning because his respiratory rate was high and he was doing a lot of “belly breathing.” He seems more comfortable now that they increased his ventilator suppport.
They also increased his morphine. Since Tucker has seen so many narcotics in the past, his tolerance is higher than the average kid. We are increasing his meds accordingly to manage his pain.
I will be honest, this has been a longer and more difficult surgery recovery than I think Tommy or I anticipated.
His surgeons do not seem surprised. They explained this morning during rounds that for Tucker, this was not a “typical” Nissen. Because of his medical history and his esophageal atresia, his Nissen was much more invasive and manipulative. He had an 8-hour open surgery.
Although this gave me some piece of mind and explained why we haven’t seen any “Tucker smiles” since his surgery, it makes it no less easy to see him this way.
I guess if you could just pray for Tucker’s healing and for us emotionally, that would be great. We are hanging in there, but certainly missing our boy and praying he will return to us soon.
Sunday, October 6, 2013 – 9:00 am
I think it’s safe to say we haven’t had a great 24 hours. It hasn’t been terrible, but it hasn’t been fantastic either. This morning when I called to get a report from the night nurse she said Tucker’s heart rate became elevated overnight (170s-190s) which is pretty high for him. His respiratory rate (number of breaths per minute) was also high so they ran some labs, took a blood gas, and a temp.
Everything was normal, but his heart rate continues to trend on the high side this morning. His stomach looks more distended and bloated today than yesterday.
We are in early discussions of increasing his pain management. Tommy just thinks he needs to poop….so there’s that.
All in all we are hanging in there. We definitely miss our happy, sweet boy. We haven’t seen any smiles yet since he returned from the OR on Friday. Hoping he turns a corner and starts to feel more like himself soon!
Tommy flies back to Richmond tomorrow (Monday) morning for work so I will be hanging solo until Thursday when he flies back to Boston. We are crossing our fingers for a discharge at the end of this week but that all depends on Mr. Tucker.
Saturday, October 5, 2013 – 9:00 am
Tucker’s first night post-op went well. He came back from the OR on slightly higher ventilator settings than his normal, which we anticipated as he woke up from anesthesia.
The good news is that they were able to put him back on his normal ventilator support of CPAP of 5 overnight. His oxygen requirements did not escalate overnight either. He’s right back to his little respiratory baseline, which is awesome!
In terms of pain management, the PICU team is following Tucker’s cues and giving him morphine and Tylenol as needed. He has a vertical incision right above his belly button and a central line in his left leg for IV access.
He is definitely a trooper. We are praying he gets some good rest over the weekend and is able to heal quickly. It’s tough for us to see him hurting and drugged, but we are thankful that this surgery has a much quicker recovery than his others in the past.
Friday, October 4, 2013 – 2:19 pm
Surgery is complete!
Everything went very well and the surgeons were pleased by the amount of stomach that Tucker had to do the wrap. (Often times kids that are fed through their lower intenstines like Tucker have smaller stomachs). Since Tucker was on G-tube “bolus” feeds for five months prior to his esophagus repair, they think that gave him a chance to stretch out his stomach…which was beneficial during this surgery.
Tucker will recover through the weekend and remain on IV fluids until Monday. They said to anticipate 1-2 weeks for recovery, depending on Tucker’s lungs.
Thanks for the prayers!
Friday, October 4, 2013 – 1:00 pm
Just had an update from Dr. Manfredi. Things are going smoothly and they’ve just started the wrap portion of the Fundoplication.
Part of the art of a Nissen Fundoplication is making sure that you don’t wrap the stomach too tight around the lower esophagus - which would prevent the ability to throw up in the future and may cause retching…or wrapping it too loose, which may mean continued reflux and the need to have the surgery redone.
We are praying the surgeons wrap it just right!
Friday, October 4, 2013 – 11:00 am
We’ve had one update from the OR. They placed one arterial IV line and are working on another. Hoping they make the first incision soon.
Friday, October 4, 2013 – 8:00 am – SURGERY DAY
Tucker is the first case on the OR schedule today, so he went down to the OR this morning at 7:30 am. The Nissen Fundoplication can take anywhere between 3-6 hours. His surgeons are doing this surgery “open” rather than laparoscopically since his anatomy down there is a bit different than your average kiddo.
The surgeons will also place a central line for IV access before they start the surgery. Tucker’s veins are so scarred and damaged from his extended time in the hospital that they have to do a different kind of IV for him.
We will update as we hear from the surgeons. Go Tucker!
Wednesday, October 2, 2013 – 10:30 pm
Okay dokie. An update on Tucker’s “plumbing.” Tommy wanted me to let people know that the sphincter I was referring to on Facebook was not in relation to Tucker’s butt.
My apologies for the confusion that may have caused.
So the muscle at the top of Tucker’s stomach (that should remain pretty near closed to keep food down) is open. Wide open. Which is why his reflux has been so significant and why we haven’t been able to move forward with oral feedings yet. Literally everything that goes in his stomach right now shoots right back up. Which is no fun for anyone, especially Tucker.
Today’s findings confirmed the need for the Nissen Fundoplication on Friday. We don’t know an OR time yet but will post it once we get that info.
In other news, Tucker’s anastamosis (site where his two esophagus ends were connected) looks great. The tissue is healthy. His esophagus is open. Very little stricturing. Woot.
Wednesday, October 2, 2013 – 10:30 am
We made it to Boston!
The ten-hour drive from Richmond to Boston was relatively smooth and uneventful. Tucker slept like a champ the entire ride (from 8 pm – 6:30 am) and woke up in Boston his happy, chipper self. Tommy and I are still catching up on sleep but thankful for a safe trip and the prayers that were sent up on Monday night on our behalf.
Tucker was admitted inpatient yesterday afternoon and will remain inpatient until he is discharged after surgery. Tucker has handled the transition well and was excited to see some of his old primary nurses from the NICU yesterday when we stopped by the unit to say hello.
It definitely feels strange to be back in the hospital. Normal and strange all at the same time. Overall, we are bigger, stronger, healthier (and wiser, more experienced) since our last time in Boston. So that feels good. To be back in Boston and know that we can be home with a thriving child. The question still remains how long will we be here….
Tucker is headed down to the OR this afternoon at 2:45 for some evaluative procedures to check out his esophagus, his reflux, his swallowing, and whatever else they decide to look at when they take him down there. What they see today will determine whether we move forward with the Nissen Fundoplication on Friday.
Will post an update later this evening once we have results to share.
Saturday, September 28, 2013
Both Tucker and I (Ellie) have head colds (fingers crossed this is NOT RSV for Tucker). Not great timing with our trip to Boston scheduled for Monday, but so far Tucker has handled things pretty well. We are on Day 4 of whatever this is.
Aside from a snotty nose and requiring more suctioning out of his trach, Tucker has not run any fevers and has been acting very much like his playful, happy self. So far this virus does not seem to have settled into his lungs. We saw his pediatrician yesterday and we will check in again with her Monday afternoon.
The game-changer for the trip to Boston will be if he develops a fever, goes up in his need for oxygen, or can not maintain his typical oxygen saturations (94-100). We are fortunate to have Tucker’s primary nurse with us today (Saturday) who is excellent, and we have a night nurse here tonight and tomorrow night….so we will all watch Tucker closely over the rest of the weekend.
Game plan is still to leave Monday night and drive through the night to Boston. If Tucker gets worse and this bug moves south into his lungs, those plans may have to change. Fingers crossed, his symptoms will start improving over the next 36 hours.
Monday, September 16, 2013
An update on plans for Boston….
- We are leaving two weeks from today (Monday, September 30th) and driving through the night to Boston. It’s about a ten-hour drive from Richmond to Boston. We’ve done a couple of shorter road trips with Tucker but this will be our first big one. Fingers crossed he will sleep through the night (he typically does), and we won’t hit any traffic on the way there.
- Tuesday, October 1st Tucker will be admitted into the PICU at Boston Children’s for some routine GI procedures to assess his esophagus, stomach, and reflux in general. Since Tucker is still on the ventilator, he will stay in the PICU until he is discharged after he recovers from surgery.
- Tucker’s Nissen surgery is scheduled for Friday, October 4th.
- Estimated length of trip: 1 – 2 weeks, but that all depends on Tucker’s recovery.
Tuesday, September 10, 2013.
Last update was Friday, August 9th. Apparently we are now on a once per month blog update schedule. Yikes. To those of you who continue to check the blog on a routine basis (namely our moms), thanks for hanging in there with us.
We’ve been in a bit of a lull, but things are about to ramp back up here again real soon so stay tuned.
A quick recap on August…
- Tucker went to the nutritionist for a height/weight check. He grew a bunch in length over the summer and lost some weight since his hospital discharge in May (a combination of actual weight loss and edema from steroids finally leaving his tissues). This was one of the goals for the summer; when the nutritionist told me in June that Tucker was clinically obese, I thought she was mean, mean, mean! But seeing him now, so much more active and healthy (and still plenty chubby) – he really does look like a different kid.
- Tucker continues to make great strides towards weaning off the ventilator. Fingers crossed we will start some “trach collar trials” (i.e. time off of the ventilator later this fall).
- Tommy has fully transitioned into his new career as a real estate agent with Hometown Realty. He is doing great and staying busy with showings, open houses, and listing appointments.
- Ellie is enjoying staying home full-time with Tucker. She spent a good chunk of Tucker’s naptime during the month of August on a “Glee” binge after Cory Monteith died on Tucker’s birthday.
- Check the esophagus for narrowing or strictures.
- Assess reflux.
- Probably get a Nissen Fundoplication.
- Consult on a corrective arm surgery.
Friday, August 9, 2013
Our week in photos….
A couple of stats on Tucker since I think we forgot to mention them in our last post.
- At Tucker’s “12 month” well-baby appointment, he was 29 inches long and 21 lbs. He grew an inch and a half since his June appointment and lost a pound (which was the goal).
- Tucker’s current pressure settings on the ventilator are 10/6. He came home on pressure support of 13/7. We have one more “step down” on ventilator support to make next week and then we hope to start trach collar trials (time off of the ventilator) this fall.
- Tucker is still on “j-tube” feeds for the bulk of his caloric intake. Although Tucker can swallow and eat, his reflux is still significant enough that we are beginning to discuss the necessity of a Nissen fundoplication surgery to help manage the reflux.
- We are also in the early stages of discussing havingTucker’s radial aplasia surgery done this fall in Boston. Fingers crossed it will be a much shorter stay than last time, and we may try to combine it with the Nissen surgery if we can.
We really hope to minimize Tucker’s time in the hospital, since Tucker has taken off developmentally since being home.
He is behind on some gross motor skills from what we refer to as “a year of hospitalized bedrest,” but we have been blown away by the progress he has made over the last two months.
When we first came home at the end of May, Tucker had such a “low activity tolerance.” Meaning playtime on the floor was usually pretty short and resulted in frequent naps.
Now, Tucker is on a typical nap schedule and has so much more energy and spunk.
The biggest surprise has been that Tucker is talking up a storm. One of our biggest fears when we faced the decision to “trach” Tucker was that we would be “taking his voice away.” I remember the first month after we trached him, I watched him cry and it broke my heart because no sound came out of his mouth.
Even though Tucker’s trach tube is still “cuffed” (meaning there is a seal of ventilator pressures inside his trachea that seals off air from passing over his vocal chords), Tucker has figured out how to make noise around his cuff. It is literally music to our ears. It’s so sweet to hear his little voice again – and to see him take joy in hearing himself speak is amazing.
And….it took most of the summer, but we got Tucker’s “new” helmet today. No one is too excited about the return of the helmet (especially since the orthotic company switched our design order and Tucker’s new helmet has dancing girl bears).
No, they’re not cool dancing bears like the Grateful Dead.
Fortunately, Tucker only has to wear the helmet 23 hours a day. Womp. Womp. As with most things “Tucker,” the helmet is for a season….and after the season we just came through, I think we can handle pretty much anything.
Saturday, August 3, 2013
It’s hard to believe that it’s already August! We’ve officially been home with our son now for 2 months and it’s been a fantastic two months. Tucker went in for his One-Year well baby check-up and our pediatrician was super encouraging about how well Tucker is doing. She was very positive and we were excited to learn that he’s grown 1.5″ since our last appointment and has lost a pound. He’s leaning out and getting longer which will help with his physical development.
We’ve also had our first swallow study since being home. His esophagus passed the test but his reflux did not. No surprise to us there. We intentionally came home on j-tube feeds knowing that reflux was an issue and hoping that he might outgrow it. This test is one piece of the puzzle that confirms that he’ll need another surgery, nissen fundoplication. A nissen is super common for kiddos with EA and used to be a packaged surgery alongside the Foker method. We attempted to avoid it but in order for Tucker to be able to eat orally it’s a necessary one.
So, we’re beginning to talk/plan a return trip to Boston in October to knock out two surgeries. The nissen fundoplication and also Tucker’s arm surgery. The arm surgery will consist of a wrist centralization and a pollicization of his index finger. Since Tucker is missing his radius bone this will center his wrist onto his ulna bone. And since he’s missing his thumb, they’ll rotate over his index finger to function as a thumb. As much as we love Boston, we’re hoping this time around it’ll be a shorter visit. Now that we’ve been able to experience life at home with Tucker, we’re already apprehensive about the idea of being back in the hospital. We’re praying now for this part of the journey and that it’s quick and painless. Thanks for praying along with us.
Now, time for some fun recent pics;







Monday, July 22, 2013
We have had a fun and busy last week. Tucker turned “one” on Saturday, July 13th. We celebrated by baptizing him at our church that Sunday, and having family over for a little birthday party afterwards.
We were excited to finally baptize him in front of friends, family, and a body of believers that has been so incredibly faithful to our family through out Tucker’s journey. Our pastor even flew up to Boston for the day to visit while Tucker was inpatient there. It was such a sweet culmination of the miraculous work the Lord did in Tucker’s life (and our lives, too) during Tucker’s first year.
Our talented sister-in-law, Sarah Lynn, took photos of both Tucker’s baptism and his birthday party.
I snagged these photos from Grandma Terry – thank goodness for family! Tommy and I definitely rolled out of the driveway and realized on our way to church that we didn’t bring a camera!
Saturday, July 13, 2013
365 days and 21 pounds later, our brave boy is 1. Here is a video recap of Tucker’s First Year.
Tucker’s First Year – 365 Days and 21 Pounds Later from Tommy Sibiga on Vimeo.
Monday, July 8, 2013
Tucker took his first road trip to Virginia Beach on Thursday, and a second road trip to our family’s lake house on Buggs Island Lake on Saturday.
Both trips went great. We felt so grateful for the opportunity to introduce Tucker to some family members who had been waiting to meet him for (almost a year now!) Tucker went in the pool for the first time at his Uncle Ted and Aunt Nicole’s, and he took a little nap on Uncle Stevie and Aunt Cat’s pontoon boat at the Lake.
Simple things that seem so ordinary….but they meant the world to us. That we are finally here. Finally, we are in season where we can live life with a fullness that we never knew in the hospital.
Our sister-in-law Sarah took some family photos of the three of us at the Lake on Saturday night and she showed me some of the initial shots she got. We look stupid happy. Our life is far from uncomplicated, but we are already doing things with Tucker that I never thought possible. And for that we are immensely grateful.
Tucker’s first Fourth of July in Photos…..
Sunday, June 30, 2013
Our apologies for the lack of updates…..there’s no real excuses other than we’ve just been enjoying our time home with Tucker. Our time has been consumed with looking at him, playing with him, caring for him, and simply being a family together. Ellie jokes that he’s hit a bit of a developmental burst this week where he’s been way more engaging, extra happy, and really making some strides on being able to sit up on his own. It’s so fun for us to see him constantly happy and sweet natured. We’re less than two weeks away from his 1st birthday and it’s amazing to think about all that he’s been through and all the ways that he’s changed and developed in just one year.
Here’s some other things that have happened since our last update; Tucker now has 4 teeth popping through, doctors cut his calories by 20% and he appears to be getting lean and long, we had an awesome homecoming party for him surrounded by friends and family, he’s experienced church, restaurants, graduation parties, Home Depot, and malls, he’s learned to kick his feet and that if he stomps loud enough on the pack and play that we’ll come over to him, he’s learned to make his own few noises even with the cuffed trach, and he loves to laugh.
This is a special video for us that we’ve kept private until now. Tucker has a cuffed trach. That means that we’ll put sterile water into a balloon that seals his trachea so that the air pushed into his lungs goes down but can not come back up. So when the cuff is inflated, no air can go up above the trach site and pass by his vocal chords. Noise/speech is created by air vibrating the vocal chords. If we deflate the cuff, some air is able to go up pass the trach site, pass his vocal chords, and out his mouth. In this video, we deflated his cuff, and this is the first time that we have ever heard his voice. Ellie can’t help but tear up every time she hears this precious noise.
Tucker’s First Time Laughing and Hearing His Own Voice from Tommy Sibiga on Vimeo.
Tuesday, June 11, 2013
Electricity is a good thing. Especially when you have a kid who is on life-sustaining medical equipment. We figured that out real fast when we lost power for 24 hours on Sunday night.
Pretty much every piece of equipment that Tucker requires has some kind of battery life, but that battery life lasts eight hours at the most…then the batteries have to be recharged. Our sweet neighbors brought over their fantastic generator as soon as we lost power on Sunday night, which enabled us to keep Tucker “plugged in” and oxygenated without burning through all of our spare oxygen tanks. Needless to say, Tucker didn’t notice much of an issue, but I don’t think his parents slept much that night.
The only difference Tucker did notice was the lack of AC. We joke that Tucker wilts like a petunia in the heat. Naturally, our best option was to leave him naked.

Overall, life at home has continued to be a wonderful transition for Tucker and for us. We have never seen Tucker so joyful and happy – he definitely knows he is home. The consistency of having two parents as his primary caretakers, plus being able to get him on an actual “schedule” have been great for his development.
At this point, we have continued sleeping in shifts since we only have one night nurse on the schedule each week, and one nurse friend who volunteers for part of the night on Friday nights. I would say nights continue to be the most challenging for us, and the most exhausting. We are hopeful that we can get some additional night coverage soon.
Here are a few pics of the our last week with Tucker at home….

Thursday, June 6, 2013
Life at home has been AWESOME! Tucker has been doing really well and appears to be settled right in. He’s happy, comfortable, smiley, and from a health-perspective doing great. We’ve taken him on several walks around the neighborhood, out to Home Depot (naturally), and back to MCV for one of his first follow-up appointments.
Tomorrow we head back to meet with our pediatrician for the first time.
We’ve also had Early Intervention Services stop by our house for an assessment and to work on some Occupational Therapy and Physical Therapy. The lovely ladies were really please with how social Tucker is. It’s been so fun for us to have visitors stop by and meet/play with Tucker while laying on his play mat or other fun normal baby activities.
For us…we have loved being home. For the last 10.5 months, we’ve had to shower, put clothes on, get ourselves ready for the day, plan/schedule the rest of the day, drive to a hospital, park, check-in, check-in again, ask the nurse how his night went, and then take a peek at him. NOW, we take a few steps out of bedroom, pop our heads over his crib, and see his smiling face beaming back at us! It’s the best.
Tucker arrived home with a lot of medical supplies and machinery but each day we’re getting a system figured out. We’re becoming a little more organized and learning how to move about the house and how to transport him around. We haven’t “arrived” yet, but it’s quickly becoming second nature.
We feel so blessed and fortunate to have found some really great nurses. They love Tucker so well and have been a great help/resource for us throughout the day.
For this week, we’ve had a nurse every day Monday-Friday. Since being home we’ve only had one night nurse work a full shift and another nurse graciously volunteer to stay til 3am.
Night nurses are still a tremendous need. At this point, we have one nurse committed to Sunday nights and one nurse committed to float for one other night a week. So we are 2/7 on the nights.
Whenever we don’t have a night nurse, we split the night and sleep in shifts. Sometimes we can sleep soundly next to Tucker and other times, alarms are going off at the exact moment of nodding off to some decent sleep.
We couldn’t be happier being at home, with our son, with our dog, as our family. We’d love to have you meet our little man, so feel free to connect with us and stop by. We would also love if you would continue to network and pray for night nursing.
Saturday, June 1, 2013: Life at Home
In case you missed this little video yesterday, here’s the homecoming video we posted of Tucker’s big day on Thursday. Shameless plug, our talented sister-in-law, Sarah, took all the photos and helped capture our day. You can see more of her work here: Photos courtesy of Sarah Lynn Saunders: sarahsaundersphoto.com/ or here: https://www.facebook.com/pages/Sarah-Saunders-Photography/194685740604380?fref=ts.
Tucker’s Homecoming from Tommy Sibiga on Vimeo.
So “life at home”….. we have waited a long time to create that sub-tab.
It has been such a joy and relief to finally have Tucker in our home. He has been happy, playful, and lively – we can already tell he is going to thrive! His first two nights at home he has slept well (he is actually still asleep as I type).
We have had nursing coverage during the day Thursday and Friday, and a sweet nurse-friend came Friday night and watched Tucker so we could get some sleep. We are still in search of night nurses for Monday, Thursday, and Saturday evenings from 11-7 or 10-6 pm.
A few people have asked about meals for our family while we adjust to having Tucker at home. My mom created a “Take Them A Meal” calendar. The recipient last name is Sibiga and the password is “Tucker.” Here’s a link as well: http://www.takethemameal.com/meals.php?t=KSNE4992.
Have a great weekend! We can’t wait to enjoy ours as a family.