Boston Updates
BACK IN RICHMOND!
Monday, May 27, 2013
Tonight for pretty much the first time in six months, I am finally sleeping in my own bed.
Our house is still littered with boxes and medical supplies, but we are here and we are home and I think I’m finally starting to feel grounded again.
Tucker’s discharge is planned for Thursday.
Tommy, Lyla, and I moved back into the house today.
The contractors are coming early Tuesday morning to finish some various odds and ends, and Servpro will come in behind them to clean and help put our house back together.
Tucker is doing well – smiling and laughing up a storm. His vent settings have returned to his baseline and hid oxygen requirements have actually been lower.
We decided to discontinue Tuckers mist collar trials until he is home and stable. We will try again in a few weeks once we know he’s at home for good and ready for those changes. Long story short, we were a little overly aggressive in trying to extend his time off the ventilator. Next time, we will take the mist collar trials much slower.
We have been blown away by Tucker’s little personality as we have continued to wean the last of the drugs he was on from all his surgeries in Boston.
We are excited to bring him home and see how he thrives being outside of a hospital environment.
We are literally counting the hours until our family can be together in our home for the first time in almost a year.
Monday, May 20, 2013
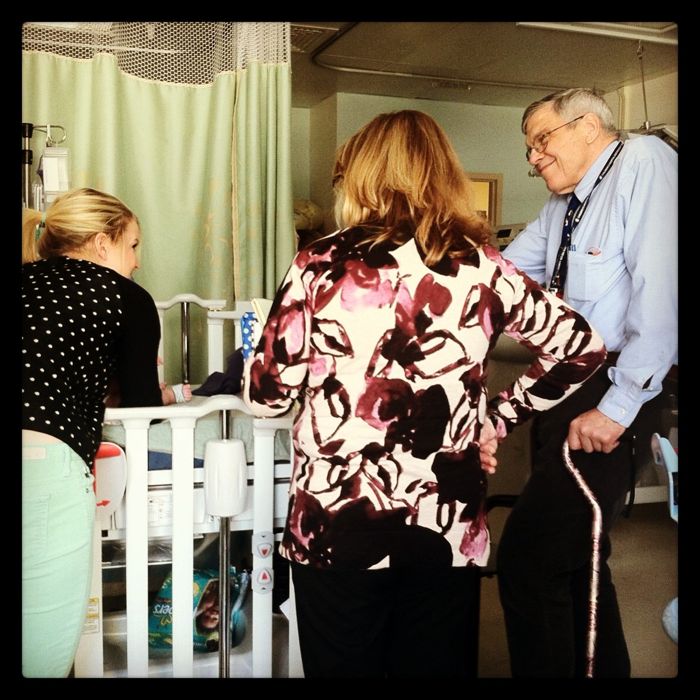
Tucker made a little move down the hall today to the step-down unit, because he no longer needs ICU level care.
He will spend the next week there until we discharge home after Memorial Day.
Tommy asked me if I was excited about the new change of scenery and I shook my head.
A new team of doctors. Another set of nurses and respiratory therapists.
Truthfully, we are just so exhausted and so done with our time in the hospital.
While we feel confident that waiting until our house is livable again and Tucker’s nursing coverage is better established is the way to go, both of us are eager for normalcy, for a routine, for a chance to live life as a family outside of the hospital.
If you could pray for fortitude and perseverance over the next week, we would appreciate it.
Pray that Tucker stays healthy. Pray that the contractors finish our home on schedule. Pray for night nurses – we still need them!
Friday, May 17, 2013
Sorry for the lack of updates. We have been working hard to find nurses and meet with contractors as they continue to repair the water damage in our home.
We are still in the PICU at MCV.
Tucker is stable and ready for discharge; however, after a lot of consideration and discussion with doctors, we decided to wait until May 27th to discharge back home.
That’s the first week we are can have a relatively full week of home nursing scheduled.
It’s also the first week that we are able to move back into our home.
We feel that the extra ten days in the hospital will allow for a smoother transition home the second go-round, knowing that we can have support lined up for Tucker’s care, and that Tucker’s long-awaited homecoming will be in his home.
In the meantime, the pulmonary team is taking advantage of Tucker’s time back in the PICU by doing mist collar trials.
Mist collar trials are where Tucker is not hooked up to the ventilator. Instead, he breathes on his own through his trach with some oxygen “misting” or blowing over top of his trach opening through a mask attached to a hose.
The goal is to get Tucker to the point where he is only on the ventilator at night and on mist collar during the day.
They were hoping to accomplish this goal by the end of the summer. Yesterday, Tucker did a total of 8 hours on the mist collar during the day, so we are thrilled at his progress ahead of schedule.
Being on a trach collar at home will also make Tucker’s care during the day simpler and more manageable, so this is great news for the next time we bring him home.
Saturday, May 11, 2013
Since Tucker is back in the PICU for a few more days (no talk of discharge plans yet), we are trying to take this opportunity to recruit more nurses for when Tucker goes home again.
At this point we have a couple of folks willing to do some PRN (part-time hours).
We have contacted seven local in/home nursing agencies, and unfortunately no nurses are available with the qualifications needed to take care of Tucker.
At this point we are trying to piece together a team of nurse friends who would be willing to cover one or two 8-hour shifts per week.
The qualifications are the individual has to be a certified RN or LPN and has to have had experience with a ventilator.
Our total goal is 40 hours per week of help (that allows us to have an open case with Pediatric Connections so that we can continue to recruit more nurses).
Our biggest desire is 6-8 hours at night, but at this point we are eager for whatever people can offer.
We should be upfront, the hourly rate is not equivalent to that of a hospital or critical care center, but it would be an opportunity to make some extra income in home setting with a one-to-one patient.
Also, Pediatric Connections will reimburse for mileage to and from our home in Hanover County.
Our contact at Pediatric Connections who coordinates the placement of our in-home nursing said she will “do whatever it takes” to get RN friends certified and in their system to join Tucker’s team this week.
If you are interested in getting signed up with Pediatric Connections to help provide nursing for Tucker, please contact Ellie at (804) 363-3710.
Thank you!
Friday, May 10, 2013
I just got back into the PICU this morning around 8:30. I was greeted with lots of gummy smiles and a much “pinker” Tucker than we left yesterday evening.
He has pretty much returned to his baseline and his respiratory settings are trending back down.
I think it’s safe to say he sufficiently scared the bejesus out of us on Wednesday morning, and he’s scared us many times before. Not like this.
Seeing your child code at home, especially on your first night home with him home, is terrifying beyond words. I think the image of Tucker lifeless and blue is one that will be permanently imprinted on both our minds for a long time.
As I was bagging oxygen into his trach, I kept praying, begging “Lord, we aren’t going to go like this. After everything we have been through, this is not how we are going to go.”
There have been various points on Tucker’s journey where I felt like I was “willing life” into our child. I have never willed life into his little body like I did Wednesday night as I stood over his crib and bagged while Tommy did chest compressions.
We are thankful for CPR training that we got twice (in Richmond and Boston), and that Tucker responded to it and hung with us until we got to the ER.
We are trying to figure out what exactly went wrong. Tucker’s trach tube was totally clear when they pulled it in the ER. We had his spare trach lubricated and ready to swap at home, but once EMT arrived, they also felt like his trach was able to move air to lungs.
One thing the docs are checking into is whether Tucker might need a slightly longer trach tube.
Regardless, we are thankful he is okay. That we were able to act quickly and maintain clear heads. That Jesus was in the midst of the most desperate moments.
Thursday, May 9, 2013
So here’s the thing…yesterday we discharged Tucker from the ICU.
And less than 24 hours we are right back where we started.
Suffice it to say, we have had a scary six hours.
Long story short, around 3 am, Tucker began acting agitated and coughing.
I was awake and noticed his monitors began ringing off with a dangerously low heart rate. His sats dropped quickly and he became limp, blue in color and unresponsive.
CPR training quickly kicked into gear as Tommy began chest compressions and I bagged Tucker’s trach. I continued to bag Tucker as Tommy called 911. I bagged Tucker and was able to get his sats back up into the 80′s but he was still clearly in respiratory distress.
I kept bagging Tucker until the ambulance arrived and a respiratory therapist took over.
We were rushed back to the ER at MCV. After the ER docs continuing to bag and suction, they made the call about an hour later to change the trach altogether.
Tucker’s trach was patent (not plugged), but the doctors believe it may have been partially dislodged or collapsed within his trachea.
Additionally, his white blood cell count was very high so we are now waiting for labs to come back and let us know if he’s sick.
Not sure when we will get out of the hospital again at this point.
Right now we are just trying to catch out breath and let Tucker recover.
Monday, May 6, 2013
The general contractors are downstairs replacing the drywall in the kitchen ceiling as I write this.
Tommy and I did our first official “trach change” yesterday where Tommy pulled out Tucker’s trach and I put a new one in. It went great – Tucker didn’t even drop his oxygen sats and Tommy and I were way smoother than we thought we’d be.
We have one more full day of specialists consults inpatient (Tuesday) and the goal is to discharge Tucker on Wednesday….
Except we are still 0-3 on finding any available home nurses. We are prepared to discharge without home nurses lined up, knowing Tommy will have some more availability during the month of May as he transitions jobs; however, having nurses at night so that we don’t have to sleep in shifts with Tucker (and for the peace of mind of Tucker’s medical team) is important.
If you know of any home nurses in the Richmond area that would be willing to work with our family, please let us know! The individual needs to have experience with a child on a ventilator within the last six months.
You can email me at elliesibiga@gmail.com. Thanks so much!
Saturday, May 4, 2013
Last weekend in the hospital? Most likely!
Tucker’s enjoying his new private room at MCV and he is loving meeting new doctors and nurses as they stop by and enter his room. He’ll greet you with a stare and a raised eyebrow as he wonders why you’ve entered his room. Our new friends from The Pediatric Connection stopped by yesterday and brought a load of new supplies and equipment that will come with us during Tucker’s discharge. They walked through a large amount of hands-on training with us and they plan to come back Monday to finish our training. They also switched Tucker over to his take-home ventilator. So far, he is doing awesome on it! His oxygen requirements are still a little high for discharge but we’re hoping that they’ll come down within the next few days.
The home oxygen concentrator only goes up to 40%, soTucker needs to be on 40% oxygen or less to be considered safe for discharge. Right now he’s hanging at 45%, so please pray that he can achieve this goal comfortably, otherwise it will prolong our time in the hospital.
Reflux. We’ve had some issues with managing Tucker’s reflux since arriving at MCV that I think we now have a good handle on. Tucker experienced sensitivity to a slight change to some comparable reflux meds. We’re now switching him back to the exact ones he was on in Boston.
Nursing. As predicted, lining home-care nurses proves to be our most difficult challenge. The hospital wants us to have a large majority of nursing hours fulfilled prior to discharge and we’re having trouble finding an agency that has the staffing needed. There are a lot of folks working on this for us, they just need to find the people who have the availability. If you know of any night nurses (maybe 10pm-6am?) out there who have at least 6 months experience with ventilators….let us know. We’d love to connect.
Discharge. Up to this point, surgical rounds and conversations have mentioned a goal of discharge for Monday (May 6th). The nursing piece might not make that possible. Tucker’s oxygen needs also may hold things up. Conversations are now moving towards a Tuesday discharge. We’ll see how it all plays out but we’re very optimistic that at some point this week we will be “home” with Tucker.
Our home. Our house is in full-on demolition mode. The walls and floors are moisture free and we’ve been given a green light to reconstruct. Our contractor’s crew should begin putting it all back together on Monday. Our plan is to stay in our house until Tucker is discharged and at that time we’ll move over to our friends’ house. Once again, this is not TLC’s “Bringing Home Baby,” but we’re so eager to finally be with our son in a home environment. Our new living situation is a really sweet set-up and we’re so excited to live with some friends.
So….the prayer requests are; oxygen levels, nursing, a quick discharge, and a fast, thorough home repair
Thursday, May 2, 2013
Rick Warren said the ultimate test of faith is not how loudly we praise God during happy times, but how deeply we trust him during dark times.
No doubt, we have felt like we are being tested “heavily” this week right as we approach the finish line of Tucker’s 9.5-month medical journey.
(In case you missed our update earlier in the week, a water valve to our upstairs toilet broke and flooded part of the upstairs, including Tucker’s nursery, and the majority of our downstairs kitchen and foyer). A contractor came and demoed Tommy’s hardwood floors, a lot of carpet, and a large portion of the drywall in the kitchen on Tuesday. He also shared with us that we need to be out of the house for at least 3.5 weeks to allow them time to replace everything that has been water damaged.
Tucker’s discharge is tentatively planned for Monday, so as you can imagine – the irony in all of this is that the week we finally get to celebrate his long-awaited homecoming, we are homeless.
Fortunately, some good friends who live nearby with a lot of square footage offered us their home yesterday. We shared with them that we are aren’t an “easy ask,” and that taking us in also comes with an entourage of home-care nurses and medical equipment for Tucker. They reassured us that they are willing to let us live with them regardless. They have two open bedrooms upstairs and an upstairs living area. They also live walking-distance to a big shopping center with a grocery store and several restaurants, so we are looking forward to being able to take Tucker out in his new stroller and around their neighborhood.
Speaking of our little man, he’s been doing great since his arrival back in Richmond. His transfer was uneventful and easy. The only time he needed more oxygen was when he had a major blow out in his carseat while we were up in the air. The six-passenger medical jet is tiny (much like a puddle-jumper), and the smell was enough to knock all of us backwards. I think the crew could have used some oxygen of their own.

The transition to MCV has been seamless, too. MCV and Boston Children’s did a ton of correspondence the three weeks prior to our transfer. MCV was so well prepared for Tucker’s arrival. Everyone has been on the same page about the goals for his time there: getting introduced to the specialists who will care for him here, and working towards a discharge. We have felt grateful for all of the coordination and conversations that took place to get us here.
Now we just need to work towards getting “home,” even though home doesn’t look like we thought it would initially.
This scripture has never felt more true for our family than this week:
6 For God, who said, “Let light shine out of darkness,” made his light shine in our hearts to give us the light of the knowledge of God’s glory displayed in the face of Christ.7 But we have this treasure in jars of clay to show that this all-surpassing power is from God and not from us. 8 We are hard pressed on every side, but not crushed; perplexed, but not in despair; 9 persecuted, but not abandoned; struck down, but not destroyed. ~ 2 Corinthians 4:6-9

BACK TO RICHMOND!
Tuesday, April 30, 2013
Tucker’s bags are packed and ready to go! The transfer team is scheduled to arrive between 9 – 10 am this morning. We estimate that will put us at MCV between 1 and 2 pm.
We will update later this afternoon once we have landed.
If you could also pray for our family – we have some really terrible water damage throughout our house that will likely mean us being “homeless” at the time of Tucker’s discharge. Obviously this timing is really unfortunate and devastating for the three of us.
We have had several offers of places to stay, and if you could pray for grace as well as traveling mercies today we would appreciate it.
Saturday, April 27, 2013
A couple more details on our next 72 hours.
Tucker’s transfer is currently scheduled for Tuesday morning at 10 am.
He will be transported via medi flight back to Richmond, and the flight is about an hour to an hour and half long. Although Tucker was born at Henrico Doctors (and we love that hospital), Tucker is being transferred to the PICU at MCV. That way, we can get him in their system at Children’s Hospital for future visits, and we can connect with the pediatric specialists out of MCV who will be apart of his care team in Richmond.
Timeline….
- Sunday (tomorrow) late morning – Tommy will leave Boston and drive our car back to Virginia. Please pray for safety on that 10 hour drive for him.
- Ellie will stay in Boston through Tuesday morning and travel with Tucker on the flight.
- Once Tucker arrives at MCV, Tommy and I will need to interview home-care nurses, continue our trach care training, and get organized at home for the influx of medical supplies and equipment that will be delivered. We hope to bring Tucker home from MCV within a couple of weeks, but at lot depends on how quickly logistics come together and how Tucker does post-flight. (Transfer can be stressful for little guys like Tucker).

Friday, April 26, 2013
4:30 pm
Tucker is back from the OR and his esophagus looked great. Dr. Manfredi didn’t even need to dilate. He did do a measurement of Tucker’s esophagus diameter and he said its 12.5-13 mm, which is now that of a baby with a normal esophagus.
Which means……we are scheduled for a medi flight back to Richmond on Tuesday morning at 10 am. Happy Birthday to Tommy!
2:00 pm
Tucker went down to the OR at 2 pm this afternoon. This dilation is our ticket home, depending on how it looks. Will update again once he’s back.
Thursday, April 25, 2013
So Tucker has tracheitis. Womp womp. Basically that means he’s got some bacteria growing inside of his trach and that’s why he’s been a little less himself the last couple days and required more frequent suctioning.
Fortunately, his nurses are all over it and started him on antibiotics right away on Tuesday night.
This shouldn’t affect his transfer next week, but his dilation tomorrow will. Whether or not his esophagus looks healthy and wide open in the OR tomorrow directly affects whether he will need to stay in Boston for another dilation, or if we are ready to go.
Please pray for a nice, open esophagus with no leaks at the connection site and minimal scarring.
We are excited!
Tuesday, April 23, 2013
Tucker’s hospital to hospital transfer is tentatively planned for next Tuesday or Wednesday. We have a lot to cover and take care of here in Boston (including another dilation on Friday), but holy moly we are talking about coming home!
Please please pray that Tucker stays healthy over the next week and that there are no “esophagus surprises” when he goes down for his dilation Friday.
He’s needed more oxygen today, had increased “chest junk” and his white blood cell count has been up today…all signs that he could be fighting an infection.
We are so eager to get him home and be together as a family in Richmond again. Please pray that we are able to take this big step towards home next week!
Friday, April 19, 2013
9:30 pm
Lots of rejoicing, relief, and cheers around Boston tonight! So proud of the service men and women who sought to see this day end in justice. Happy to be back with our guy at Children’s this evening. We will sleep well tonight. What a day!

9:00 am
Quick update. Tucker had a pretty good day yesterday and a great night. His withdrawal symptoms have lessened and we have been able to wean his vent settings fairly aggressively. He’s gone from 27/7 @ 80-90% oxygen down to 18/7 @ 45% 16/6 @ 35%. This is amazing news and we think his respiratory status will continue to improve in the days to come. They’re planning on taking him off one of his last remaining big drugs (Precedex) today or tomorrow. We’re hoping that this will have a significant impact on his overall mood and pressure requirements. Every day we pray for the Lord to meet our needs and to have His hand displayed in Tucker’s life! Praise be to God that He answers.
We received a date for Tucker’s next dilation (final one before leaving?). He’ll go down on Monday, April 29th for a look at his esophagus and maybe another one or two procedures. We’re hoping to arrange for transfer shortly after that date!!! We’ll keep you posted.
P.S. If you’re watching the news this morning, the community right next to where we are living is going crazy right now. We’re one of the districts (Newton) that’s asked to stay inside until further notice.
Wednesday, April 17, 2013
Many folks have been asking about Tucker’s transfer date back to Richmond. We appreciate your excitement and eagerness for our family to be together in one place.
Please know that as soon as we have received an official transfer date, we will share it.
That being said, we could use some prayer for the following issues:
- Tucker is on substantially higher vent support than he was post-operatively. 36 hours post-trach, Tucker was on pressure support of 18/6 with 40% oxygen.
- 48 hours post-op, Tucker’s vent needs rose to 27/7 with 80-90% oxygen.
- While Tucker’s current ventilator settings are perhaps acceptable for a hospital to hospital transfer, they are NOT settings that are safe for him to be discharged home on.
- Tucker’s oxygen needs to be below 40% to be discharged on his trach and home ventilator. Coming down on his pressure settings is also necessary.
No one seems to know why Tucker’s ventilator support rose so significantly over the weekend. The general consensus is that his lungs are fluid-overloaded after he layed in the bed for five days recovering from surgery.
The goal is to transfer him home on vent support that he is ready to be discharged on once we arrive back at a hospital in Richmond.
Since we moved forward with the tracheostomy to bring him home, it is incredibly frustrating and disconcerting that with his new trach, he is now on high enough ventilator settings that also prevent him from being safe to discharge. His respiratory needs continue to feel like a battle that we cannot win.
Additionally, Tucker is experiencing withdrawal as his team once again has to repeat the drug weaning process. We’ve been through this once before, which gave us an idea of what to expect; however, seeing your baby withdraw is a difficult experience.
Finally, please pray for the training process as we learn how to take Tucker home on a ventilator and oxygen. It is a ton of information and technology management for two non-medical parents, and we are feeling pretty overwhelmed.
Monday, April 15, 2013
Surreal.
That is the only word that I can come up with to describe this day.
I am truly thankful to be safe. I am so heartbroken for what took place in this city today.
We had four friends in town from Virginia, two of whom were running the Boston Marathon. Our friends got to Boylston Street early this morning around 8:30 am to secure great seats at the finish line.
I was able to join them at the finish line around 9:30 am. We spent the entire morning watching incredible paraplegic athletes cross the finish line, cheering on the elite runners, and snapping photos of my friends’ husbands as they completed the final legs of their races.
Tucker’s nurse told us about the incredible spirit of the Boston Marathon. It was every bit as joyful as they described. There is so much hometown pride on Patriot’s Day here in Boston. People turn out by the thousands to cheer on strangers and neighbors alike.
I kept texting Tommy as I was walking up and down Boylston Street this afternoon, telling him how much I wished he were here in Boston. I wanted him to experience the pride of this city today. The energy was so amazing, so genuine, so full.
My friend Lisa’s husband crossed the finish line around 2:15 pm. We left our chairs at the finish line and walked down Boylston two blocks to meet up with him.
Fifteen minutes later, the first explosion occurred, about 25 yards from where we had been sitting.
I was underground on the T headed back to the hospital when the first explosion went off, and I think I caught the last train outbound before the MBTA evacuated the subway completely.
As I got off the Longwood Medical stop for Children’s Hospital, ambulances began rushing down Huntington Avenue from Brigham and Women’s Hospital back into the city. I saw people on the street slack-jawed, staring at their phones and asking strangers what was going on. The fear was palpable.
I think that is what hurts my heart the most. The fear that is permeating this city tonight stole joy from what began as such a beautiful day. Evidence that the world we live in is so deeply broken.
As I left Boston Children’s Hospital around 6 pm, I noticed an armed guard stationed at every door in the main entrance. I made eye contact with one of them, wanting to say “I am so sorry that you have to be here.” He looked down at the ground and half-smiled back at me, with such sadness in his eyes.
Please pray for this hurting city tonight. It’s not our hometown, but we love it like its ours.
Sunday, April 14, 2013
Tucker’s having a few rough days recovering from his tracheostomy surgery. He doesn’t like laying in bed with limited mobility (who does really?). We’ve tried using minimal sedation so that he’ll be able to wean off all the drugs more readily. Keeping him still continues to prove challenging, which is ultimately what allows the trach site to heal. He needs to remain sedated until the first trach change on Tuesday.
In the meantime, we’ve been reading and researching about what life will look like when we get home.
We’ve been asking a lot of questions, and folks have been asking us a lot of questions….so I thought we’d share some of the information that we’re finding out;
The Not So Fun Facts About Tucker’s Tracheostomy
- Timeline;
- Tucker will most likely spend the next year on vent support 24 hours a day. So at all times, his neck will be hooked up to the ventilator (breathing machine) for pressure support and likely supplemental oxygen as well.
- Spring of next year (2014), we will hopefully be able to switch over to a trach collar during the day (i.e. no tubes hooked up to his neck) and potentially just need vent support at night while sleeping.
- Two years from now (Spring 2015), we will hopefully be able to decannulate (remove the trach and allow for Tucker to breathe through his mouth normally).
- Schedule. While Tucker is on vent support….at all hours of the day, we will need someone who is awake/alert to respond to alarms that are affecting his airway. That means;
- In order for Ellie and I to sleep we either need to sleep in shifts in his nursery and/OR hire home-care nursing to stay in our home at night while we sleep.
- If we want to leave the house, we will need two adults in the car at all times. Someone will have to sit next to Tucker in order to respond accordingly. So during the day, Ellie won’t be able to leave the house and run errands unless someone drives her or is trained and able to be the one who sits next to Tucker.
- Machines. At all times Tucker we need to be hooked up to (or have with us); ventilator, oxygen concentrator, oxygen tank, pulse oximeter and monitor, portable suction, feeding pump, an extra trach, an extra g-tube, and a plethora of other medical supplies. It will be a production to go out and about. Ellie and I have to be trained/certified on using these machines. Additionally, we will have to do his trach cares once a day and replace the trach once a month. These trach cares/changes require two people to perform.
- Talking. While on vent support, Tucker likely will have a “cuffed” trach. With a cuffed tube, Tucker will be unable to make noise. We won’t hear him cry, laugh, or make other typical baby sounds. The cuffed tube doesn’t allow for air to pass over the vocal cords where sounds are made. Once he is only on a trach collar, we hope to switch to an uncuffed tube or one with a speaking valve that’ll allow for him to start making noises.
- Eating! Tucker has never been able to take oral feedings. With a trach, he’ll now be able to try a bottle. We’re hoping in the next week or two he can try his first oral feeding ever.
- Water. We’ll have to be especially careful around water since Tucker’s trach is an open airway. We’ll have to be protective of it when it comes to bathtime and other bodies of water.
Friday, April 12, 2013
Before

Immediately After

Now-ish (almost hard to see where the trach comes out because of his double chin fat)

Thursday, April 11, 2013 – Tracheostomy Day
10:00 PM
So Tucker has a trach.
The surgery went fine, minus a few episodes of oxygen desaturations thanks to Tucker’s “reactive airway” and chronic lung disease. At least, it affirmed to Tucker’s surgeon and everyone else that his chronic lung disease is significant enough to warrant the tracheostomy.
Tucker is now stable and on a cocktail of narcotics, several of which are the same drugs he was on for his esophagus surgery.
I tried not to have a visceral reaction when they brought him back up from the OR and I saw the tower of med pumps we worked so hard to get rid of two months ago. Fortunately, this time those drug drips will be short-lived. But seeing him sedated like that is an image that I would like purged permanently from my memory after next week.
I would like to say we were instagramming the heck out of Tucker’s face post-op, but the reality of seeing him with two new tubes coming out of his neck was a little sobering for both of us. It is one thing to reconcile with a trach intellectually, and another to see your child hooked up to a ventilator that will likely breathe for him over the next year.
So we didn’t take pictures. We just kissed him, and scratched his head.
Then we walked up the street to the Regal Cinemas at Fenway Park to see a movie – during most of which I suppressed tears.
When we walked over to Tasty Burger afterwards, I broke down crying next to a bar full of half-drunk Red Sox fans.
And that was our day. Tomorrow some good, honest pictures. We promise.
9:30 AM
Tucker is down in the OR as I write this…and when we took the elevator down to the surgical waiting area and kissed Tuck goodbye, it was the first time I felt myself get teary before sending him off.
Because we know he’ll come back up different than ever before. That we won’t hear his voice for a while, that we will revisit that haunting experience of seeing him deeply sedated for several more days.
This is the surgery we never wanted and knew inherently that he always needed.
The surgery itself is routine and fast, but the lifestyle implications are unique and months long. It is in the very truest sense, a bittersweet surgery for us.
I mentioned that last week was a week of “holding on and letting go for us.” I think the reality is the last eight and a half months have been a season of holding on and letting go.
Letting go of normal, of what we believed babyhood to look like. Letting go of our expectations, experiences, desires and plans for Tucker. Letting go of what Tucker’s life should be like in our eyes, and surrendering that expectation to Jesus completely.
In some ways it has been a grieving process for us, and in that wake of grief we have experienced grace and trust in a way that is so deeply abundant and simple.
So here we go, anchored to hope, a new chapter begins.
Wednesday, April 10, 2013
Tucker heads down to the OR tomorrow (Thursday morning) at 9:15 am for his tracheostomy. Pray for a smooth surgery and fast wean off of pain meds (this is the thing that probably worries us most). We’ll update tomorrow after his surgery.
Friday, April 5, 2013 – Dilation Day
I think this was the most nervous we have been walking into a dilation. Starting Sunday, Tucker’s g-tube drained a significant amount less than normal and he began to wretch and hock up some loogeys (secretions) a lot more frequently. We were worried that his esophagus suddenly began to stricture/narrow. Now that we’re making plans to come home on the respiratory side, we were scared that the esophagus was going to be what keeps us in Boston.
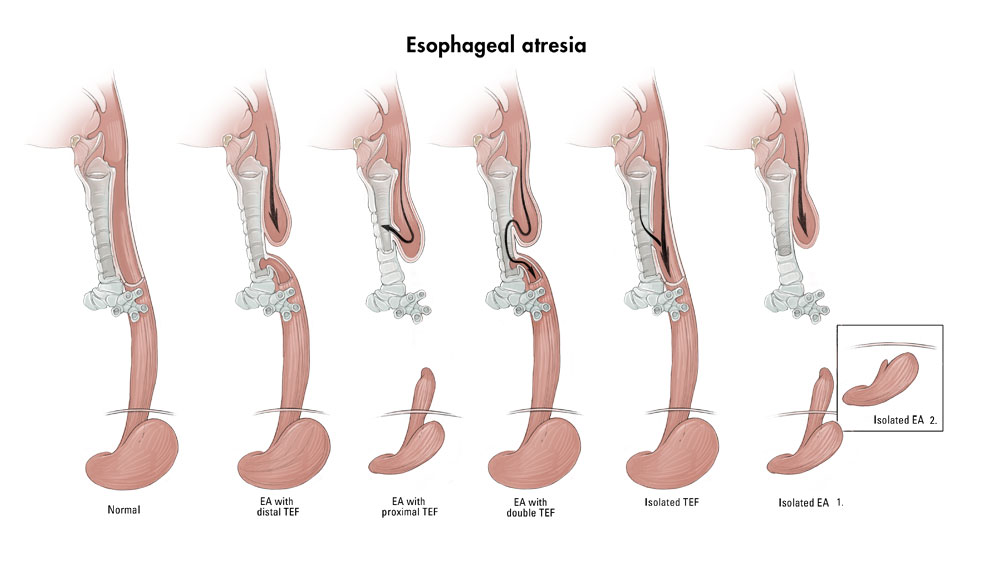
Well…after a several hour delay to build the anticipation, Tucker went down for his dilation. Words can’t express how relieved we were when the surgeon came back and said his esophagus looks great! He said it looked wide open and almost decided to leave it alone but chose to dilate it to 12mm (our end goal). He’d like to take a look at it in a month (or before we leave Boston!….whichever comes first). It’s been two months since his esophagus connection and we are so amazed by the success of the Foker procedure. Please keep praying for the health and healing of this vital body part.
Dilation today and a tracheostomy on Thursday (April11th) and we’re on our way to making HUGE strides HOME! We’re in conversations with several case managers to figure out the logistics of getting home. The plan that is most likely is to take a medi-flight and transfer to a Richmond hospital. Once in Richmond, we’ll spend several weeks in a step-down unit and allow for doctors/nurses to get to know Tucker. Additionally, it’ll allow us time to receive training on operating the ventilator, performing his trach cares/changes, and begin conducting interviews for home-care nursing. We’re hoping that’ll be a very quick process and asking for prayers that logistics are smooth and fast! Apparently finding home-care nurses to work night shifts is the hardest part of this all, so we’re praying specifically to find some excellent nurses that are excited to take care of our man.
The first chapter of Tucker’s story is almost closed and we’re so appreciative of all the folks that have been reading along and have had their names written next to his cheering him on. Thank you!
Wednesday, April 3, 2013
Monday afternoon we spoke with Tucker’s pulmonologist and let him know that we were prepared to move forward with a tracheostomy for Tucker. He said he was sad for us and for Tucker and he was sad for himself because he had to be the one to break the news to Dr. Jennings (Tucker’s esophagus surgeon who does not like trachs). Haha.
He also said he thinks we will see a big difference for Tucker, and later told us that Dr. Jennings took the news just fine. I think at this point everyone is in agreement that Tucker’s lungs need time to get healthy and the best place to do that healing is at home.
So onward we go…Tucker’s fourth (and maybe last?) dilation while inpatient is scheduled for this Friday, April 5th. They’ll also do a rigid scope of his airway and evaluate the level of any possible tracheomalacia.
If you think of it, please pray for Tucker’s dilation this Friday. Tucker has been more symptomatic of some strictures this week, and we are hoping that his esophagus is in the same place it was last time Dr. Manfredi dilated it (11 mm with minimal strictures as the connection site).We really need that million-dollar esophagus to cooperate so that we can go home after Tucker’s tracheostomy.
Tucker’s tracheostomy is scheduled for next Thursday, April 11th.
Here is our blue bunny himself, who could not have been more thrilled that we put him in a hot, itchy suit on Easter.
A little happier here (like we said, he prefers nakedness).
Sunday, March 31, 2013 – Easter
Shortly after our last post, we needed to increase Tucker’s respiratory support to 6 liters of high-flo. Another indicator for us that Tucker’s respiratory course will be a long one. Another realization that’s been on our minds as we’ve been weaning pressure settings is that we can look back now and notice that Tucker is less happy, engaging, and awake. The weans have been “acceptable” but is he “optimal?” We’re feeling that the best option for Tucker is to move forward with a tracheostomy and get him home.
When we arrived in Boston in November, we became friends with another couple whose son shared the bed space next to Tucker’s in the NICU. Their beautiful son was discharged about a month ago after receiving a trach. We reached out to them and asked them if we could invite ourselves over to see what life looks like with a baby and a trach. They graciously allowed us to come over and spend an entire night watching and participating in their nightly routine. We left feeling overwhelmed by all the equipment, and a bit intimidated by the care that we’d have to provide for Tucker, knowing that our lifestyle will look atypical than most of our friends for the next couple of years.
Still, we were filled with an amazing HOPE for Tucker’s future/development, an EXCITEMENT to be in our home to take care of our son, and a CONFIDENCE that the Lord has chosen us to be Tucker’s parents and will equip us with everything we need to give him the fullest life possible.
We wouldn’t have to worry about whether he has enough lung reserve/energy to sit-up, learn how to crawl, roll around on the floor. Tucker would have as much oxygen as he needs until he’s a little older and has outgrown the lung disease from being a preemie. It would mean we could still bring him home in May or June, rather than this fall or an indefinite timeline. A trach is a short-term solution, and it would most likely come out when he’s 2.
It’s not the way we envisioned leaving Boston this Spring, but we are reminded again that God is writing a different story for Tucker – and we have to trust that His story is the best story.
So….that’s where we’re at. It’s been a week of holding on and letting go for both of us.
We’re planning on talking to our team tomorrow to begin the planning and scheduling of things. This a big decision that’ll commit us (and Tucker) to a very different way of living…..please pray that we will continue to feel at peace about moving forward.
Thursday, March 27, 2013
Tuesday afternoon we ended up going back up to 5L of high-flo….a step in the wrong direction but one that we all feel is what’s needed to test and determine what Tucker’s lungs can currently handle. On 5L, Tucker is much more consistent in his sats, more awake during the day, and is able to better tolerate wearing his helmet and splint. We’re excited to have him be in a happy place and to continue working on developmental milestones.
We met with a very large team of folks yesterday to ask questions, clarify acceptable sats, and to explore the possibilities of the next step for Tucker. A large majority of the conversation was centered around a tracheostomy. It’s a huge decision for us with lots of intimidating unknowns. We asked a lot of questions about what life looks like with a child and a trach. We gathered some really great information and are planning to reach out to a family we met in Boston that went home on a trach. We’d also like to visit a rehab center and see what that experience would be like. The end result of the team meeting is that we are going to slowly try to wean Tucker’s pressure settings over the next several weeks and in mid-April meet together again and see if he’s made progress. Our prayer is that by April 15, he will have been able to comfortably wean to 3L of high-flo. If he struggles to get down, we’re praying for confidence in our decision to move forward with a tracheostomy. Pray for tucker to “declare himself.”
In other news, we have officially began to give Tucker a big boy bath. This is a big deal for us. When he was smaller, nurses would fill a small Tupperware tub and place him in it every once in a while but he’s been too large and too heavy for many months now. So we went out and bought him a tub that we can sit on his bed and that he can sit up in. He’s been pretty good already about sleeping through the night and we think this new nightly bath time routine will help even more. It’s quite the operation, but we’ll try and get a picture of it tonight.

Tuesday, March 25, 2013
Just when things were looking up….we hit a road block. Nothing major at this point but definitely something that puts us back on an indefinite timeline.
As (somewhat) expected, Tucker wasn’t able to handle the last wean in his respiratory pressure settings. On Saturday, they weaned his high-flo down to 3 and he had a fairly decent day. Going into the night and into the morning it was apparent that it was too much, too fast for him so they bumped him back up to 4. The plan is to now leave him at 4 and try him again at 3 on Monday. Rather than trying to wean him every other day, we’re going to try one wean per week (on Mondays). If he’s not able to do one per week, then we’ll increase the spacing between weans until we figure out what he can handle. It could be he needs a full week, it could be he needs a full month, or it could even be he needs several full months. We won’t ever really know until we try. Thus becomes a very indefinite timeline.
Until Tucker gets down to a low-flo of 1, he’s not allowed to come home. At the same time, if the only thing keeping him in the hospital is respiratory support, then he doesn’t really require the intensive care that Boston Children’s offers. So, nurses and doctors are beginning to discuss with us options for the next step.
If Tucker is not able to wean his pressure settings in the near future we basically have two options….we can have a tracheostomy and go home fairly soon or we can avoid surgery and transfer to a rehab center. A rehab center provides all of the respiratory support required but in a less hospital-like atmosphere. Ellie and I are both committed to pursuing the rehab center route. That then leads to the question…a rehab center in Boston or Richmond??? And then of course, how long will we be in a rehab center? Which the answer is “nobody knows.”
We’re trying to be optimistic that Tucker will make it down to 1 and could use all the prayer that we can get to see that come to fruition in the near future. Praying for healed lungs and our family to be home (in our house) in Richmond. Thanks for joining with us in asking for Jesus to be in the midst of Tucker’s life.
Saturday, March 23, 2013
Whew! What a busy week.
Tucker turned “5 months old” on Thursday. Tucker’s due date was October 21st, 2012, so we use his “adjusted age” to track growth and developmental progress. His nurses and doctors say he is pretty developmentally appropriate despite his prematurity and the fact that he was under heavy sedation for 5 weeks.
Tucker has had many visitors, including the guru of Esophageal Atresia, Dr. Foker, who invented the surgery that changed Tucker’s life and gave him a complete esophagus. I don’t think this man will ever truly know the depth of gratitude we feel for his role in our son’s life. It was a joy to see him yesterday and he was very pleased with how healthy Tucker (and his esophagus) looks.
We had our scheduled meeting with Tucker’s medical team on Friday morning. No major decisions were made other than to regroup in another two weeks to see what kind of respiratory progress Tucker has made. Tucker is currently at 4 liters of high flow on his nasal cannula and he needs to wean 1. They are planning to wean to 3 today, if all goes well.
There was some concern raised after Tucker’s dilation on Wednesday because the anesthesiologist said that the short window of time Tucker’s oxygen cannula was out of his nose, he “pretty much dropped like a stone” in terms of his oxygen saturation. So I think there is some concern that Tucker will be able to wean down to 2 or 1 liters before the end of March. Please, please continue to pray for Tucker’s lungs. The best cure for chronic lung disease is time, but it also means extended time in the hospital…and if Tucker is unable to wean down appropriately, the question of trach is still out there.
On a good note, everyone is in agreement that Dr. Foker and Dr. Jennings “worked a miracle” and Tucker’s esophagus looks exceptional!
Wednesday, March 20, 2013
Happy First Day of Spring! Boston celebrated the start to spring with six more inches of snow yesterday, with more on the way on Thursday. We loved the snow in December, January, and February, but at this point this Virginia girl is ready for some warmer temperatures. Sheesh!
Tucker had a good day. His auntie Jill is in Boston for a few days so she came and snuggled Tucker and hung out with me in the surgical waiting area while Tucker was in the OR.

Tucker’s dilation went well. Dr. Manfredi dilated his esophagus to 11 mm. (He dilated it to 10 mm last time, and it had narrowed to between 8 – 9 mm since Tucker’s last dilation 10 days ago). The goal is an esophagus diameter of 10-12 mm, so we are well within the desired range.
Dr. Manfredi was very pleased with how Tucker’s esophagus tissue looks, too. He said the tissue looks really healthy, and that there is very little stricturing or scarring. He has been injecting steroids into the connection site every time he dilates Tucker’s esophagus and he feels like that is really helping to smooth out any scar tissue in Tucker’s esophagus. Dr. Manfredi said we can anticipate 1 – 2 more dilations before discharge.
The results of Tucker’s hearing screening were an improvement from his initial hearing test. The audiologist said she still thinks he has some degree of hearing loss, but it’s more mild (as compared to moderate hearing loss in January). He will have another hearing screening in a month or so to determine whether or not the hearing loss requires any kind of intervention down the road to help with language development.
We have a meeting scheduled on Friday morning for 7:30 am with Tucker’s pulmonalogist and the Esophageal Atresia team to talk about benchmarks for discharge. Woot.

Tuesday, March 19, 2013
In case you missed last Friday’s post, Tucker has acquired a new accessory in the form of a helmet. No, he does not have a brain injury. It’s to help round out the sides and top of his head from laying in the hospital bed for such prolonged amount of time. Helmets are awesome. Google them – the before and afters are incredible.
Here Tucker is in his helmet from yesterday.
My parents got him that onesie. It took him approximately 35 minutes to poop through it and return to nakedness…which is why he is naked in most of his pictures. (I’m sure he will thank us for that some day). But seriously, the kid doesn’t care about clothes. He either blows them out or sweats through them, so at this point I am wondering whether we just need to settle for “naked Tucker” who wears only a diaper and his helmet.
Several people have commented on his rolls and asked for a weight update. Tucker weighs somewhere between 17-18 lbs. Boyfriend is a chunk. Praise the Lord for that chub. Being with him every day, I have started to take his chub for granted. I forget how desperately we prayed for that chub in the beginning. His chub is nothing short of a miracle.
All in all, he is doing so incredibly well. I am actually crying as I type this because I am overwhelmed with thankfulness. The resounding comment among nurses and doctors in the NICU is “He looks SO good.” “He’s doing SO WELL.” We still have some ground to cover, but it is incredible to see him growing leaps and bounds, developmentally and physically.
Tomorrow he goes down at 11 am for his third esophagus dilation and a repeat hearing screening. If you could pray:
- That his dilation goes smoothly and that there are no leaks or complications that result from ballooning the connection site.
- That Tucker’s repeat hearing screening shows no sign of hearing loss. After his initial hearing screening, the audiologist told us Tucker has some moderate hearing loss, which Tommy and I (and many of Tucker’s nurses) feel is not the case. We are praying for better and more accurate results than the last screening.
Monday, March 18, 2013
Lately.
What’s been happening lately….
- Tucker’s team weaned his nasal cannula to 5 on Saturday. They’ll wean to 4 tomorrow, assuming all continues to go well. “1″ is the magic number.
- Emi and Grandad (Ellie’s parents) are in town for a visit until Tuesday.
- Tucker goes down for his third dilation on Wednesday and a repeat hearing screening.
- Tucker won his very own “MVP” award at the City Church banquet in Richmond last night. He accepted his award via Facetime to a very kind audience (and some of his biggest cheerleaders), who sang him “Jesus Loves You.”
- Ellie’s sweet friend Ginny and her husband Mark gave birth to their new son, “Jack Marshall” on St. Patrick’s Day. Congratulations to the Evans family. We LOVE you!
Friday, March 15, 2013
Tucker has graduated back to high-flo. He’s been handling the switch well and is at a high-flo of 6 right now and the doctors will wean him to 5 on either Saturday or Sunday. We’re hoping Tucker cooperates and that each week we’re able to make significant progress on reducing his respiratory support. If everything goes as planned….Tucker could reach the required settings needed for discharge by the end of March (strictly from a respiratory standpoint). Pray for his lungs and that they get stronger and healthier every day in order to handle these adjustments.
A new piece of Tucker’s fashion apparel will be dropped off today. Tucker will be wearing an orthopedic helmet for the next several months to help round out his head. There’s some mild head molding from being in a hospital bed for so long and now is the only time to help correct it (while the brain is rapidly developing and the skull is expanding for it to grow). The helmet is strictly for cosmetic purposes and he’ll wear it for about 3-4 months.
From a drug standpoint, they’ve been able to wean his methadone some and he’s currently experiencing some mild withdrawal from the last decrease. What that looks like for us is that his heart rate is a little higher than normal, he’s a little more irritable and jumpy, and he often wakes up a little gaggy and retching. Not a big deal but enough that we can tell a difference. We’ve given him an extra day off from weaning and will likely wean again today. It’s important for us to keep these drugs out of his system but we also want to make sure that it doesn’t impede his respiratory progress.
While still in the hospital we’re hoping to really work on some developmental milestones. Yesterday we stuck him in a Baby Einstein activity seat for the first time. We had to prop him up with some blankets and he eventually settled in and seemed to like it. It was fun for us to see his chubby legs just hanging there. Hoping to keep getting him out of bed and allowing for his core to strengthen. He’s almost grasping at rings and we are also hoping the activity seat will help develop these motor skills.
Home is in sight and we’re so excited to bring Tucker home and have you meet him and love him. Thanks for being in this with us!

Tuesday, March 12, 2013
It was a busy weekend/start to the week for Tommy, Tucker, and me. I flew home on Saturday for the first time since Thanksgiving, while Tommy stayed in Boston for the weekend with Tucker. Tucker had a GREAT weekend with his dad. Lots of fun playtime, good sleep, and they were able to wean his CPAP to 5 on Sunday, which he tolerated beautifully.
Since his respiratory requirements are essentially what’s keeping Tucker in the hospital, it’s crucial that Tucker is able to continue weaning on his oxygen. He started at a CPAP of 8, weaned to 7, to 6, to 5 on Sunday and today they will take Tucker off of CPAP and transition him to a high flow nasal cannula of 5. The ultimate goal is for Tucker to wean down to a low-flow pressure of 1.
The process for Tucker is to make two oxygen pressure weans per week, depending on how well he handles them. This week, he’ll need to go from high-flow pressure of 5 to 4 a the end of the week, then 4 to 3 next week, 3 to 2 (low-flow), then hopefully 1 by the end of March.
In other news, the team from plastics came back to take some more measurements for Tucker’s helmet. Tommy and I got to pick out a cute blue helmet with cars and flags on it for Tucker, which will come in at the end of the week. He will wear it for about 3 months to round out his head from laying in a hospital bed so much.
I am heading back to Boston this afternoon and Tommy will fly back on Thursday. I am excited to see my little guy later tonight!
Friday, March 8, 2013
Tucker went down to the OR today for his 2nd dilation. Prior to going down, we asked the doctor what would be the ideal result. He said the best case scenario would be that his esophagus has remained around 8mm and that we are able to dilate to 10mm. Well….guess what? The suture site looked great and he was dilated nicely to 10mm. Praise the Lord for His mercy to us. They’ll let him rest for a bit and take him down again in 10-14 days.
In other news, we met with a consultant for Plastics the other day to take a look at Tuckers head to determine if a helmet would be able to correct his head shape from being born so early and laying in bed for so long. During examination there was a small concern that his skull sutures have prematurely closed (craniosynostosis). Today, they took X-rays of his skull and the report came back that things look normal. They will come back later and fit him for a helmet that he’ll wear for approximately 4 months.
While taking X-rays for his head, they also took some of his right arm. We’re beginning to meet with an orthopedic surgeon to hear about a possible treatment plan for his arm when the time comes.
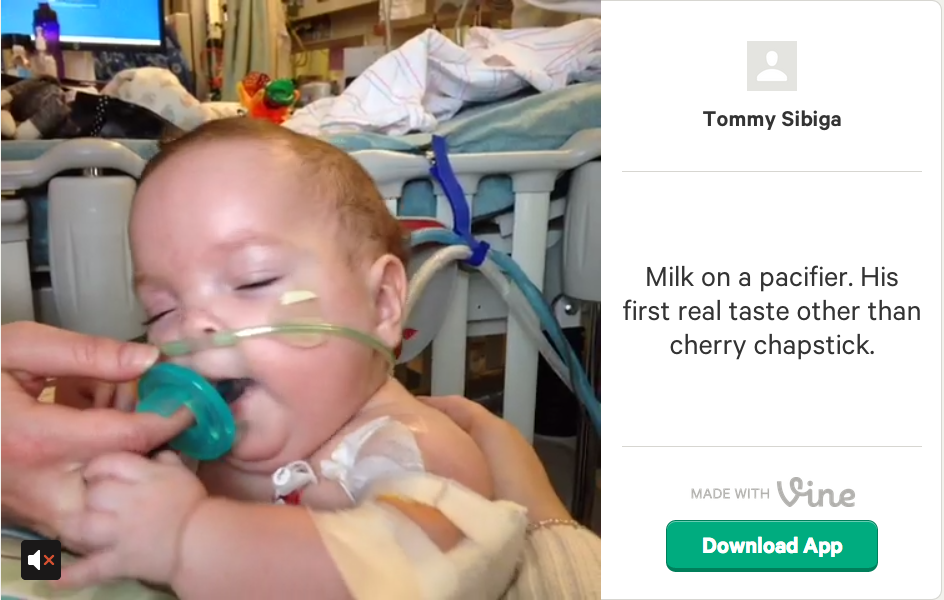
Tucker also had his first taste of milk yesterday. Check out this video to see his excitement. http://vine.co/v/bHV0mxMDvOw
The plan for the week is to wean him down to a CPAP of 5 on Sunday and at some point switch over to a high-flo of 5 later this week. Once over to high-flo, we may be allowed to have Tucker try out a very small bottle of milk. Woot!
We’re very excited about this news and praying that it keeps coming!
Wednesday, March 6, 2013
We have had a busy couple of days here in Boston! Tommy returned to Richmond on Monday, and our sweet friend Kelly and our sister-in-law Sarah flew in yesterday from Richmond to visit this week. Tommy’s boss and Regional Director for Young Life, Scott, is also in Boston for the week and came by the hospital Tuesday afternoon to visit Tucker. Yesterday was a full day of touring around Boston and Newton – which we ended with dinner in the North End at Antico Forno and dessert from Mike’s Pastry. I think we all feel asleep last night in a food coma.
Tucker has had a decent couple of days, considering all of the changes that we are continuing to make with his drug weaning and CPAP pressures. After his team shut off his Midazolam on Sunday (the last of his”big gun” drugs before Methadone), he has shown some moderate signs of withdrawal but is hanging in there. Yesterday, they converted his Methadone from IV fluid to Methadone given through his G-J tube. We are trying hard to ditch that PICC line in his arm so that we eliminate the risk for another blood infection (hopefully by the end of this week).
They also weaned his CPAP pressure to 7. Next step is to wean his CPAP pressure to 6, then once he reaches 5, switch him to a high-flow nasal cannula. Lowering Tucker’s respiratory settings is key to getting him home. And if we can get him off of CPAP, maybe we can actually take him for a spin in this stroller around the hall.
Tucker is scheduled for another dilation this Friday. (Dilation #2). Tomorrow (Thursday), Tommy flies back into Boston. Tomorrow morning we will meet with Tucker’s whole medical team (surgeons, pulmonalogist, NICU attending(s)) about the benchmarks needed for Tucker to be discharged, as well as a preliminary timeline. (Postponed til next week due to attendance) This is exciting and also a little nerve-wracking for us. The word “going home” has rarely been used for us the last seven months, so tomorrow’s meeting is certainly a milestone.
Sunday, March 3, 2013
Tucker is officially off of Morphine and Midazolam (Versed). As a result, yesterday he was fairly grouchy, his oxygen requirements were higher, and he slept for most of the day. He frequently woke up fussy and needed to be consoled. It’s been a little taste of normal parenting skills for us; trying to figure out what he likes and doesn’t like, whether he wants to sit up, suck on his pacifier, is he too hot, too cold, etc. Additionally, we’re trying to discern his cues for signs of withdrawal or irritability. The Midazolam was just turned off last night at 10pm, so we’re hoping to get through the worse of it this morning and get into a good spot by this evening.
Some happenings for the week ahead;
- Lower Tucker’s CPAP pressures through the course of the week. We’d love to get Tucker back onto a high-flow nasal cannula. This week will be the first real opportunity to get a clear picture of the trajectory of the healing of his lungs. Up until this point, he’s either been on a high dosage of drugs, fighting an infection, and/or having other assaults onto his lungs. We’re praying for some miraculous healing of his lungs. Tucker needs to make huge strides in terms of weaning of flow pressures and oxygen percentages.
- We’re also hoping to wean his Methadone down slowly. This will be a slow taper but we’re hoping to make progress each week.
- His next dilation will be on Friday, March 8th. We’re praying that his esophagus has maintained the 8mm dilation and that we can move forward little by little. It’s likely that we’ll need a minimum of 5 dilations before surgeons feel comfortable with a discharge.
- Speaking of discharge….we will meet with Tucker’s medical team later this week to talk through the benchmarks and milestones that Tucker needs achieve prior to hospital discharge. We’ll possibly talk about a timeline as well…..which is a little dangerous because there are so many variables that could alter/change the timeline. One doctor mentioned getting Tucker ready for discharge by April, maintaining him in the NICU for a month, and then discharging him locally in May. We’ll bring him home to our apartment in Newton for a week or so and then make the drive HOME (home)! Again, this is hypothetical, but I thought it worth mentioning for others to join us in praying accordingly.
Friday, March 1, 2013
9:30 am – Post-dilation #2
Tucker’s dilation went well. Dr. Manfredi said Tucker’s esophagus had narrowed a bit since his dilation last week, so he was glad they decided to take him down to the OR today to dilate. They used steroids and an 8 mm balloon to widen his esophagus at the connection site.
Tucker likely will go down to the OR again next week for another dilation. Hopefully after the third one, we will have a better sense of how many he will need prior to discharge.
7:30 am
Tucker is in the OR this morning for his second dilation. He was the first case on the schedule, and Dr. Manfredi said the procedure will take about an hour.
The width of Tucker’s esophagus at the last dilation a week and a half ago was 9 mm, which meant it was open/wide enough that they didn’t feel the need to dilate.
The goal width for swallowing solids is 10-12 mm. We will see how things go today and update later this afternoon.
Wednesday, February 27, 2013
Monday we finally took the big step of weaning Tucker off his Midazolam and Tuesday he was right back on it. Apparently, he didn’t handle the last wean too well and after several boluses during the night, the decision was made to put him back on and try again at a slower rate. He didn’t seem to mind and by the time I flew in….he was in an awesome mood.
Two great things have happened in the last few days; Tucker has regained his love for his pacifier and he’s been super excited to sit up and look around for hours at a time. We’ve had a great couple days holding him, playing with him, doing some physical therapy with him, and trying to pull some smiles out of him.
We’ve got a new plan for his pain meds. Currently they are increasing his Methadone dosage to compensate for cutting off his Morphine tomorrow morning. They’ll allow him a day or two to settle in with that and then cut his Midazolam down to 0.025 for a day and then hopefully cut it off the following day. Once he’s off Morphine and Midazolam, it’ll be a long and slow taper for the Methadone.
Tucker will be going down to the OR on Friday for a dilation. We’re praying that his esophagus has maintained the expected 9-10mm and that he handles his first dilation with flying colors.
Saturday, February 23, 2013
You’re my back bone,
You’re my cornerstone
You’re my crutch when my legs stop moving
You’re my head start,
You’re my rugged heart…
Phillip Phillips – Gone, Gone, Gone
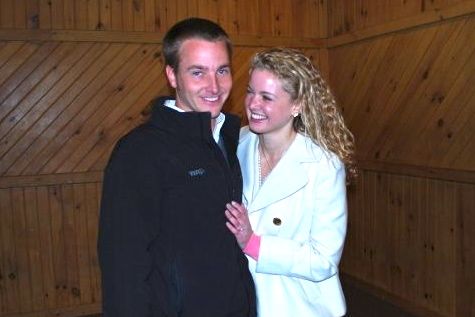
Four years ago this weekend, this handsome guy got down on one knee at Young Life’s Committee/Leader Weekend and asked me to marry him.
I was 23. I had no idea what marriage was about. I had no idea what I was about.
{Not that I pretend to now}….
But I can say that after four years, particularly the last seven months since this little guy arrived, I have never felt more grateful that Tommy and I are in this life together.

Today, I am in Boston with Tucker and Tommy is at Committee/Leader Weekend back in Virginia. While I am sad to miss time with friends and incredible Young Life leaders, I am mostly appreciating the significance of this weekend in our lives and our marriage. It was the beginning of a journey that neither of us anticipated, but we have experienced richly what it means to become a family as a result.
So if you see my husband at Committee/Leader Weekend this weekend, please don’t pity him for our circumstances.
We love Jesus and we love each other more because God made us the stewards of an incredible child.
Thursday, February 21, 2013
A quick recap of the last 48 hours:
- Tucker was extubated Wednesday morning and went back on the bipap mask for 24 hours.
- Tucker’s team was able to wean his bipap support significantly last night; as a result, Tucker’s respiratory team switched him back to CPAP (less support than Bipap) this morning. He has been doing great on CPAP thus far.
- Tucker had an echocardiogram and an eye exam to check and make sure the yeast found in his blood did not spread to those organs. Both his heart and his eyes looked normal. Praise the Lord.
- Tucker did have to go back up slightly on his drugs from the intubation on Tuesday. We are hoping that will get back on track with his weaning plan tonight (Thursday night).
- Tommy is back in town for a brief 24 hours visit (Thursday morning – Friday lunch) before heading back to Richmond. Happy momma and Happy Tucker!
Tuesday, February 19, 2013-Procedure Day
I’m back in Richmond but the report that I got from Ellie contained the words pristine, exceptional, and normal. So far, we’ve received great news and I’ll let her chime in later on today with more details.
The ORL doctors scoped his airway and said it looked pristine. There was a danger that his subglottic stenosis was a contributing factor in the lack of respiratory improvement and that it was going to need surgical intervention. Instead, they said his airway looked normal apart from the diverticulum site….which they said is healing nicely.
In his esophagus, Dr. Manfredi was hoping to perform Tucker’s first dilation with a 6mm balloon and a goal of eventually getting the diameter of his esophagus dilated to about 12mm. Instead, Dr. Manfredi said that his esophagus looked exceptional and that it was likely 9-10mm on it’s own. They decided not to dilate this time around and allow it to continue to heal.
They finished off by placing a new PICC line and switching over to a G-J tube.
Later up today is an echocardiogram and an eye exam to look for yeast concentrations? (I think that’s what they’re calling them) So far they’ve found some patches in his kidneys and liver, checking to see if the infection has spread any where else. Praises for an awesome report concerning his airway and esophagus and prayers for the antibiotics to fight this infection fast.
Monday, February 18, 2013
We have had a relatively quiet day. Tommy and our sweet friends the Havasys left early this morning, and Tucker and I were sad to see them go. Part of my day included going to see “Safe Haven” by myself at the Regal Fenway, since there’s nothing like a good Nicholas Sparks movie to induce a much-needed ugly cry.
Tucker is hanging in there on BiPap. Still pretty tired and feeling crappy from his blood infection, but he seems more comfortable than he did yesterday. Bipap appears to be giving him the respiratory support he needs right now as he is fighting off this infection.
Tomorrow at 9 am, he is going down to the OR for several things:
- The placement of a G-J tube. This will allow Tucker to start getting milk again (yay)! Tucker has had a Gtube since he was a little guy, but now that his esophagus is connected, he refluxes a lot of his stomach contents. A “G-J” tube feeds food into his jejunum (part of his lower intestines), which prevents acid reflux affecting his “connection site” as it continues to heal.
- A bronchoscopy. This will be a quick procedure to evaluate Tucker’s subglottic stenosis in his airway. “Subglottic stenosis” is essentially a narrowing of Tucker’s airway caused by prolonged periods of having a breathing tube down his throat. Depending upon how severe the swelling/narrowing is, Tucker’s surgeon may want to go in and fix that narrowing.
- A central IV line. Since Tucker’s PICC line had to be pulled on Saturday due to the blood infection, they have just been using two peripheral IV lines, which don’t last long especially since Tucker is an active fella. A central line will stay in longer and will prevent them from having to stick Tucker as many times as they did yesterday (12 times yipes).
- Pray that this blood infection doesn’t spread to Tucker’s other organs. It can spread to his heart, and his eyes. He will have an eye exam and an echocardiogram later this week.
- Pray for fast healing and improved respiratory support.
- Pray for peace, courage, and sanity for Tommy and me. We are feeling really worn down emotionally and physically.
Sunday, February 17, 2013
Well….another sucky day. The hospital called us this morning to let us know two things; his respiratory has gotten worse and they were switching him to Bi-Pap (with the potential of reintubating at some point today) and that they found yeast to accompany the bacteria in his blood infection. Additionally one of his IV lines went out and various nurses and doctors have been poking him all day to try and get a new line in. Since he has an infection, they took out his PICC line, which means he needs two IV lines at all times to inject all the meds/fluids that he is currently on. So at this point they have to constantly decide whether to give him nutrition, antibiotics, or pain meds until they are able to get a second IV line. Needless to say…all three of us are worn out. We’re praying hard that the new micro-fungal antibiotics begin to work immediately so that his respiratory support requirements decrease to the point that we can avoid being reintubated and return to CPAP or high-flo. We need the antibiotics to start kicking butt and fighting off this infection…ASAP.
Saturday, February 16, 2013
Some answers. Yesterday was filled with Tucker being generally grouchy, a high heart rate, and intermittently running a fever still. During the morning they took an X-ray of his arm and found a fracture in his upper humorous and they took some additional X-rays this morning to investigate further. That could explain the heart rate if he were in pain but it doesn’t explain the fever. His respiratory requirements were also elevated so they were still questioning possible causes. The surgeons wanted to rule out a leak in his esophagus before entering into a long weekend so they took him down for another esophagram. We were so thankful to find out that his esophagus looks as it should and that there is no leak. After this test and all the recent activity, Tucker was worn out and couldn’t quite bring himself back together from a respiratory front…so they needed to increase him to a CPAP of 10. He then slept for most of the day/night. At the end of the day, one of his tests finally came back positive indicating an infection in his blood. Although its unfortunate he has an infection it was good news for us to have a possible answer to all his symptoms. They’ll fight the infection with antibiotics (which he’s already been on since Thursday morning as a precaution). Praying he’ll recover quickly and be ready for his first dilation, a bronchoscopy, and his new g-j tube that’s tentatively scheduled for Tuesday. Also praying to see that smile again soon.
Friday, February 15, 2013
Hindsight is always 20/20. So next time Tucker is due for infant vaccinations, I will go with my gut and tell the attending to please hold off on shots until we are not two weeks post-op, and trying to wean off narcotics. Call it parental instincts, but I shoulda seen this one coming.
Yesterday started off like a normal day for us….waking up at 6:30am to call the hospital and see how Tucker’s night was. We hope to hear that he had a fantastic night and that there were no significant changes. Instead, our nurse informed us that he had a rough night, spiked a fever, his heart rate was up, they moved him back into the isolation room, and they were going to switch him back to CPAP. This began the typical onslaught of running several tests and growing cultures. There were several initial thoughts of what was causing the change; a leak in his esophagus, a fracture in his arm, acute withdrawal symptoms, etc. But as the day went on, he seemed to be fine other than the high heart rate and fever. They’ve been giving him Tylenol to help bring down his fever but as parents, we can tell he has been feeling a little off. I think this face probably says it all:

As of right now, the general idea is that Tucker is just feeling lousy from getting four 6-month vaccinations on Tuesday. They’ve switched over to using Advil to bring his fever and heart rate down. Apart from those symptoms, the nurse told us his attitude has been great, they gave him a bath for about an hour last night and he was loving it, and for his latest trick….he’s learned how to smile and has been giving those out generously. Before he started feeling icky, we caught a video of his big gummy grin:
Tucker Smiling from Tommy Sibiga on Vimeo.
Tuesday, February 12, 2013
“Love me. Love me. I’m not what you expected, but oh, please love me.” ~Kelle Hampton, on the birth of her daughter Nella.
One of the things I appreciate most about Tommy is the way he loves Tucker. He teaches me daily what it means to love our son in a way that is simple and uncomplicated. Tommy continues to remind me to take delight in our child, even in the most challenging of circumstances.
Posted by Ellie on Vimeo.
P.S. Tucker’s esophagram went great. No leaks, minimal narrowing and stricturing at the connection site. All in all a good report!
Monday, February 11, 2013
Day 212 in the NICU. I try not to count days that Tucker has been in the hospital, but Tommy has a ticker on his iPhone and I caught a glance of it in church yesterday and that number astounded me. We have been doing this for 212 days. Sometimes that number feels staggering and sometimes it just feels so normal that life before Tucker feels like the distant memory of another life.
Tucker has had a relatively decent couple of days since our last update. Withdrawal symptoms are still present, but less dramatic. He has been up on his oxygen support today and we’re not totally sure why.
Tomorrow he goes in for his first esophagram since his big “connection” surgery two weeks ago. We are praying hard for an open, patent esophagus with NO LEAKS! Update to come tomorrow evening with hopefully some cool pictures of his “whole” esophagus.
Saturday, February 9, 2013
And the snow just keeps comin’….I’m not sure how much we’ve got exactly – over 25 inches with drifts up to who knows how many feet. It’s enough that if Lyla were here in Boston with us, she would refuse to go outside to use the bathroom for fear of being completely buried.
We hoped to get out and get back to this hospital this afternoon, but the MBTA (train) just announced that the T system is closed down for the rest of the day. The driving ban has not been lifted for the city of Boston either so it’s looking like we’re just going to have to stay put in Newton.
Tommy is watching back to back episodes of 24 (long live Jack Bauer). I just poured my fourth cup of coffee and am catching up on laundry.
Fortunately one of Tucker’s primary nurses has him yesterday and today, so we know he’s in fantastic and loving hands.
Sounds like Tucker has pretty much just slept since we left around lunchtime on Friday. Hanging out under his makeshift tent, riding out the blizzard with his white noise-maker and Mr. Socks. I know his nurse is keeping a close eye on his withdrawal symptoms. We will check in throughout the day to make sure he’s doing okay.
Here are a few pics from last night and this morning courtesy of Tommy’s iPhone:
Friday, February 8, 2013
Our stay in Boston wouldn’t be complete without a true winter Nor’easter, so we are hunkered down in our cozy apartment riding out the storm. Anticipated snow fall is 2 – 3 feet. The city of Boston put out an ordinance banning people from driving on the road past 12 pm and the Mass Transit system is shutting down at 3. It seems like the whole city is shutting down this afternoon.
Tucker is hanging in there and so are we.
The good news is that Tucker is handling being extubated beautifully and doing great on CPAP.
The hard reality is that now that he is extubated, it’s time for all of his drips and drugs to be weaned and he is going through withdrawal.
Watching him go through withdrawal is probably the hardest part of this entire process for me as a mom, because literally I am helpless.
What does a baby look like when going through withdrawal?
Tucker is gaggy, sweaty, has tremors, and spends most of his awake time angry and crying. He doesn’t smile and his eyes don’t track as they normally do. His nurses really want to limit his stimulation, so all of his usual tricks just make him more upset or irritable. They put a tent over his bed this morning to keep out some of the sunlight and shield some of the noise from being in an open bay in the NICU.
What’s even harder is that neither of us are able to hold him. It has been five weeks (today) since Tommy or I have gotten to legitimately hold Tucker. Not holding your baby for an extended period of time is unnatural and difficult in the most positive of circumstances.
Not being able to hold him or comfort him when he is visibly upset and inconsolable is heartbreaking.
His nurses have said the weaning process will take 2 – 3 weeks. We are praying that as the drugs work their way out of his system, he will return to the happy, sweet-natured little guy we know and love.
Wednesday, February 6, 2013
EXTUBATION DAY….I am trying to find something positive to say about “Extubation Day.”
Tucker got extubated. So, that’s good. Buh-bye breathing tube down his throat.
The afternoon that followed Tucker’s extubation was not so fun.
Tucker’s team wanted to try extubating him to BPAP, which basically delivers the same number of automated breaths and pressure settings that he received on the ventilator. Except with BPAP, everything gets delivered through a mask over his mouth and nose.
After three hours of crying into the mask and acting completely miserable, Tucker’s team was ready to explore some different options.
I held him very briefly, which offered us nothing except for more tears from Tucker and the confirmation that the kid is in fact a bruiser and matches the weight of a small piglet.
Around 4:00 pm, his team put him back on the CPAP mask he was on before he got intubated for surgery.
At which point, our exhausted fella literally tuckered himself out and looked like this:
Even being back on CPAP, Tucker was settled but he wasn’t totally stabilized when I left the hospital at 8 pm. When he was asleep, his sats were beautiful and smooth. When he was awake, he was crying and agitated. And, he’s hoarse from having the breathing tube down his throat for five weeks so he can’t cry without it hurting, which just makes him cry worse.
Could you pray for us? Pray that Tucker gets more comfortable and has a good night sleep after a rough day. Pray the swelling in his throat goes down and he settles out on CPAP.
Pray for my spirit. It’s days like today that make me feel like we still have a long road ahead.
Tuesday, February 5, 2013
Tucker has had a fantastic day! He has made significant progress on weaning his settings on the ventilator…so much so that his doctors want to extubate him tomorrow (Wednesday).
We are beyond thrilled, considering that they just lifted his paralysis yesterday.
They will likely extubate him some time Wednesday morning after morning rounds and put him on BPAP, which is CPAP with a rate that still delivers breaths.
He’s not totally back to his busy self, but it is so good to see his sweet, bright eyes again. I am hoping that I’ll get to hold him tomorrow if his extubation goes as planned.
Neither Tommy nor I have held Tucker in five weeks between his being intubated, the surgeries, and the paralysis so I am itching to snuggle that little dude.
P.S. Tucker’s friend Sergio from Ireland is getting ready to go home after a long stay at Boston Children’s Hospital. Like Tucker, Sergio is one tough, courageous fella. We have enjoyed getting to see Sergio and his family around Children’s and we are so thrilled that this leg of their journey is coming to a close.
You can see a video of Sergio’s story here.
Monday, February 4, 2013
Tucker’s awake! They’ve lifted the paralysis today and so far he’s doing well. Praying for some huge respiratory strides in the days ahead.
Sunday, February 3, 2013
Quick update on Tucker. They decided not to lift his paralysis today and hold off until tomorrow (Monday) when Tucker’s full surgical team is here. He’s had a fine weekend. We are looking forward to tomorrow!
Friday, February 1, 2013
Tommy flew back to Richmond yesterday, so I spent most of the day listening to the Civil Wars and trying not to cry into my coffee cup at Tucker’s bedside.
Kidding.
Kinda.
Actually, no that’s true.
Yesterday was the start of a new schedule for Tommy. He will start flying back and forth each week from Boston to Richmond so that he can get the spring semester rolling for Young Life back at home. We have enjoyed the blessing of his flexible schedule over the last 6 – 8 weeks, which has allowed both of us to be together with Tucker the whole time Tucker has been in Boston.
I definitely felt sad when I pulled into the Children’s Hospital parking deck solo yesterday and signed in at the reception desk without my buddy.
If you could pray for us we can transition to this new schedule of Tommy flying back and forth, we would greatly appreciate it. I know Tommy is also feeling sad that he won’t be here on Sunday when they wake Tucker up from paralysis, so if you could pray in particular for Tommy being back home away from Tucker that would bless me. I am biased, but he is such a faithful, sweet dad to Tucker. My heart hurts for him that he can’t be with Tucker when he wakes up from his “two-week nap” and looks up at us with those big, blue eyes.
There’s not much to update on Mister Tucker other than they are planning to wake him up from paralysis on Sunday.
Once he’s off paralysis, they hope to start weaning him off the ventilator fairly aggressively so that they can extubate him to CPAP. They have tried weaning his ventilator pressures a couple times over the last 48 hours and both times he hasn’t tolerated that particularly well. We pray that once he wakes up from paralysis and is able to contribute some breathing on his own, he’ll require less help from the ventilator.
They took some x-rays of his arms this morning to check for fractures. Strangely enough, extended paralysis can mean lowered bone-density for the kiddos who are under it (because the kids are only receiving nutrition through IV fluids), so they are susceptible to fractures just laying there. I’ll find out later this morning when I go into the hospital whether or not he has one, but I sure do hope not.
Happy Friday! Thanks for checking in with our family and continuing to pray.
Wednesday, January, 30, 2013 – Post-Op Surgery
In case you missed yesterday’s post, TUCKER’S ESOPHAGUS IS NOW FULLY CONNECTED.
Tommy and I passed Dr. Foker on his way out of Children’s Hospital last night. I think it took a minute for him to connect the dots that we “go with Tucker,” but he said “things came together really nicely today.”
We’ve only known Tucker’s life with an incomplete esophagus.We are beyond thrilled and grateful that this is no longer our reality. Yesterday’s surgery was such a long-time coming, and Tucker’s largest hurdle yet. To have that behind us means for the first time in six months, we can make progress towards bringing him home.
A lot of people have asked what’s next for Tucker…..
The timeline for heading home is still likely several months, because we have a lot of preparation and maintenance to cover before we bring him home.
Esophagus “Maintenance” and Preparation to Come Home:
- Tucker will remain under paralysis for three to five days post-operatively to make sure the site of connection has opportunity to heal. Then his team will start a long, slow wean of all the meds and drips he has been on since being intubated at the beginning of January.
- Two weeks from yesterday, Tucker will have his first “connected” esophagram to see how fluid is moving through his esophagus. His surgeons will look for leaks, strictures, or narrowing at the site of the connection. He will likely stay intubated until February 12th, but a lot depends on how much his ventilator needs come down between now and then.
- 5 or more esophagus dilations before we are discharged from Children’s Hospital to prevent narrowing at the connection site. We think that these are usually spaced out at least one week apart and won’t start until after that first esophogram.
- Swapping Tucker’s G-Tube for a G-J-Tube. Tucker will keep his G-tube in his stomach for likely the first several years he is home with us, even if he’s not using it. They will send him home with a G-J tube, which sends his food to the jejunum (a lower place in his intestinal track) that doctors have found reduces the occurence of reflux once he starts eating. This switch will most likely take place during that first esophogram and he’ll remain on IV fluids until then.
- Possible sub-glottic stenosis repair. Tucker has some lasting swelling and damage in his airway from having a breathing tube down his throat for so long. His surgeon will likely want to do something to augment this swelling so Tucker does not have to fight with a narrowing airway to breath. There’s question concerning whether or not this will have to be performed before being extubated.
- We have no idea how this will go. We are praying that because we removed the risk for aspiration by repairing Tucker’s esophagus, fixed his diaphragm, and removed the atypical pocket in his trachea, all of those things will allow Tucker to make BIG STRIDES in weaning his oxygen needs. It’s possible that the healing of his lungs will take longer than the healing of his esophagus…so please pray for dramatic improvement in this regard.
- Here’s how the respiratory “weaning” sequence usually looks:
- Tucker is currently intubated on the ventilator and was on CPAP for weeks prior to surgery. Part of the reason Tucker’s team considered a trach was because Tucker was unable to move past CPAP. We are praying that when he is extubated in a few weeks, he will be able to make great progress.
Tuesday, January 29, 2013 – Surgery Day
This is it. Tucker has been sitting in the NICU for the last 200 days waiting for this surgery (potentially). Here’s our prayer for today’s surgery…..that the surgeons would easily be able to connect the two ends of Tucker’s esophagus together. That’s our hope. Some other possibilities are that they will either need to allow it to stretch/grow more using internal traction or that they will need to reset the sutures and put him back on external traction.
The surgery is supposed to take all day and we get updates every 90 minutes from a liaison. As we hear how things are going….we’ll update it here. Thanks for praying with us.
7:30am: Tucker’s wheeled down to the Operating Room.
9:15am: Dr. Jennings just stopped by and let us know that they are just about to begin. He’s prepped and ready.
10:30am: First incision was at 9:15am. Things are going well so far. One fun surprise is that the nurse said Dr. Foker is back in Boston and is in the OR along with Dr. Jennings.
12:30pm: Boom! Connected esophagus. Dr. Jennings just stepped out and told us they’re all done and are closing him up. He said it the two ends went together nicely and that Tucker didn’t move a hair. It’ll be another hour or so til they are totally finished but for now, we’re ecstatic.
2:00pm: Tucker returned to his bed spot looking great.
7:00pm: Celebration dinner at Cheesecake Factory.
Monday, January 28, 2013
Tucker had a smooth weekend, and Tommy and I were able to steal away for awhile Saturday evening to see Blue Man Group perform at the Charles Playhouse.
Over the weekend, there was some question as to whether or not one or two of Tucker’s traction sutures in his esophagus had torn out, which would potentially require intervention today (Monday); however, when Tucker’s surgeon came by this morning to examine his sutures and take new x-rays of the traction clips, he felt that the sutures were still intact and under tension.
And, even more positive news – Tucker’s esophagus ends are close enough that they want to take him down to the OR for surgery tomorrow (Tuesday) instead of this Friday.
Tucker’s surgery is now scheduled for 7:30 am tomorrow morning and the surgeon told us again, to plan on the entire day for surgery.
The goal of this surgery is connecting Tucker’s two esophagus ends. There also is a possibility that the surgeon could replace the external tractions or switch to internal traction, but he is hopeful that they will be able to move forward with an anastomosis (connection).
The outcome of tomorrow’s surgery rides on how Tucker’s esophagus tissue looks once the surgeons get in there, as well as how much tension his two esophagus ends will be under if they try to connect.
The more tension, the greater the chance for strictures, tears, and leaks once the esophagus is connected. The surgeons want “ample esophagus” to connect to ensure the best long-term prognosis for Tucker.
Some things to pray for over the next 36 hours:
- Healthy esophagus tissue with minimal scarring from the sutures – that the surgeons have good tissue to work with and plenty of length on either end for a connection.
- For comfort and respiratory stability throughout the surgery. It will be another long day for Tucker’s little body. We pray that he handles tomorrow’s surgery as beautifully as he handled the last one.
- For lung improvement over the next 12+ hours. The surgeon mentioned he would like to do a little “lung clean-up” today to minimize some of the wetness on Tucker’s lungs and optimize him for the OR tomorrow.
- For wisdom, skill, and discernment for Tucker’s surgical team and pain management team.
- For patience and trust for Tommy and me.
Saturday, January 26, 2013
2 months in Boston=done!
Tucker is doing great and seems to be preparing himself for the next surgery. The last few days, the surgeons haven’t stretched his esophagus and are letting it settle and “beef” up. They’ve made a few adjustments to his vent settings but its been more up and down and just averaging out. We have OR time booked for Friday but they may still bump him up if there’s availability and if they think he’s ready.
In other happenings…we got a bit of bad news yesterday. Doctors conducted his first hearing test and informed us that they believe he has moderate hearing loss. Mild hearing loss refers to fluid in the ears, ear infection, etc. Moderate is described more as a permanent type of loss. They said that he can hear all loud sounds but didn’t seem like he was picking up lower sounds. All that being said, there will be some additionally testing/screening for us down the road. We’re optimistic that it’s not that big of a deal….but please pray it so.
Thursday, January 24, 2013
Thursday! It’s hard to believe it’s already been a week since Tucker’s surgery last Friday. It feels both longer and shorter than that. Paralysis definitely stinks (that’s putting it mildly), but Tucker continues to do well and make great strides in terms of esophagus growth.
We are trying to be patient, but I have to admit I miss our lively, bright-eyed little guy. We can’t wait for the day he wakes up from his second surgery with a connected esophagus!
This afternoon, Tucker’s team took him down to fluoroscopy to do another “gap-o-gram” where they inject dye and measure the distance between his two esophagus ends. In short, they were thrilled with the results. The distance between Tucker’s upper esophagus and his lower “distal” esophagus is only 1.37 millimeters.
Here are some images of his esophagus before the Foker procedure and as of today, under traction:
It’s hard to tell, but in the first image from the end of December, his gap was about 3.5 cm long. In his image from today, the two esophagus ends are almost touching – that little note says 1.37 millimeters apart.
Isn’t that incredible? This is what we came here for. Tommy and I have both said to each other several times this week, “We’re really doin’ it.”
We have waited six months for this repair. It blows us away to think that one week from today, Tucker’s esophagus will be made whole.
The game plan for the next week remains the same. Continue stretching and coasting along the ventilator.
- Tucker’s big “connection” surgery is scheduled for next Friday, February 1st. If availability in the OR changes, they may push surgery to earlier in the week. As we have learned, plans can change very quickly around here.
- Tucker’s esophagus needs to grow a little more to make sure the connection isn’t done under a lot of tension. (The surgeons prefer there to be about 1 cm overlap of the two esophagus ends before the repair).
- If Tucker’s esophagus reaches the point where surgeons are pleased with length, they will “park it” for a couple of days early next week to let his esophagus “beef up” before the big surgery.
Tucker’s entire medical team has been so pleased with how well he is doing. One of the attending’s told me today that his ventilator settings are comparable to that of an Esophageal Atresia child without chronic lung disease during this part of the Foker procedure.
Rock on, little man. We are proud of you!
Tuesday, January 22, 2013
Tucker’s surgeons officially began “stretching” his esophagus yesterday. The first couple of days they just let the sutures set and as Tommy mentioned below, over the weekend Tucker’s esophagus ends had already moved closer together just by “relaxing into position.” We feel incredibly fortunate that Tucker’s gap is on the mild range of long gap esophageal atresia cases, because that will help minimize the length of time he is under paralysis before the big connection surgery.
In terms of lung health, Tucker continues to be smooth and stable. His ventilator pressures aren’t as low as they were pre-surgery, but that is to be anticipated after a 14-hour surgery where one lung was pushed aside and manipulated. It takes some time to let that lung heal and re-inflate. Doctors aren’t rushing him on weaning his vent settings, but following his cues and continuing to monitor his CO2 levels and title volumes (size breaths he is taking).
Some sweet friends from Richmond flew up for a three-day weekend visit. We had a wonderful time with them walking around Newbury Street, visiting the Boston Public Gardens and doing some fun Boston sight-seeing that we don’t always allow ourselves the opportunity to do when it’s just the two of us.
They flew out last night, right as the next snow storm arrived in the city of Boston.
Monday, January 21, 2013
Tucker has had a great couple days. Nurses increased some of his pain management meds to get him comfortable but apart from that it’s been a low-key weekend. Immediately after surgery, his vent settings went up but the doctors/nurses have been pleased to ween some of those pressures down as his damaged lung has recovered each day. They may start the stretching of the esophagus ends today (growth induction process). Doctors wanted to let the sutures set as well as allow the ends to relax into position before pulling on them. The ends have metal clips and each day they take x-rays to track the progress. The surgeon told us yesterday that without stretching yet, the ends are almost touching…woot! They’ll want a nice amount of overlap before going in for the connection and the time in between also allows for the esophagus walls to grow thicker. As the doctors would say “so far, so good.” We’re praying for another week or so of smooth sailing.
Saturday, January 19, 2013
First off, thank you so much for showering our family with love and prayers yesterday. Tucker did an amazing job handling all that was being done to his tiny body and we are really pleased with everything that the surgeons were able to accomplish in one very long day. The day flew by for Ellie and I. We were calm/restful and feel that was a gift from the Lord. So thanks for praying for us.
Currently, the two ends of Tucker’s esophagus are sutured and then connected to external traction. The sutures are then drawn out through his back and each day the surgeons will stop by and check the tension. Every few days, they will increase the tension which is pulling the esophagus closer together. Once the x-rays show that the two ends have began to overlap, Tucker will go back to the OR and they’ll do an anastomosis to connect the ends. Doctors believe that it’ll take about 10 days or so for Tucker’s esophagus to grow enough to be connected. During this time (and for some time afterwards), Tucker will be under paralysis and also heavily sedated. During this process, he’s at a high risk for infections, fractures, the sutures ripping out, and a few other things. Please pray for a flawless 10 or so days and that his esophagus grows together conflict-free.
So, what’s our timeline after the esophagus is connected? We were originally told that it would be 2-4 months after the initial surgery. He’ll need several dilations on the suture site over the next couple months and other complications can arise that would require additional surgeries. We’ve met (and heard) from some families that are in/out within the 2-4 months but we’ve also met some families who have been here for over a year to two. Each kid is so very different and their path so varied. For us, even after the esophageal issues…there will be a lot of progress required for his lungs to develop to the point where they’d let us come home. It’s taking us 188 days to get to the beginning of our road home. Thanks for traveling along with us.

Friday, January 18, 2013—Surgery Day!
9:23pm: And he’s back. They just now wheeled him back to the NICU. Waiting for them to get him settled so we can see him.
7:30pm: Sounds like they went for the diaphragm plication afterall. They moved us to a different waiting room and said that they probably have another 2 hours to go.
5:00pm: Our pulmonologist stopped and shared a little bit of the news that he’s heard. He heard that Tucker’s a rockstar and handling everything great, that it was a big enough diverticulum that they decided to repair it, and that the gap ended up being a little longer than expected so they placed him on external traction. They are predicting that he’ll need to be under the external traction for about 10 days. So that would mean he’ll be intubated, paralyzed, and sedated for those 10 days or so and then we’ll be right back to the OR. Once he’s connected, we’ll have to wait and see what other surgeries/procedures may be needed. This is essentially…the beginning of the beginning.
3:45pm: The two little pieces of information we received is that they started to place the traction sutures and then they also made an addition incision around his neck. So that means two things to us….1. He’s going to be placed under either internal or external traction, which means that we’ll have another surgery in the next couple weeks to go back in and connect the esophagus. 2. Seems like they decided to ligate the fistula/diverticulum.
2:00pm: Things are going smoothly and Tucker is tolerating everything well. They’re still working along and are undecided about which way they’ll proceed.
12:30pm: Not much more detail. They’re still working on separating things out and said that it’s all going smoothly.
11:00am: “Things are great and moving along well”
9:15am: First incision made
We’ll be updating this post throughout the day as best as we can. The liaison gives us updates every 90 minutes. Surgery could potentially take the entire day. There’s a lot of unknowns right now and the biggest one that you can be praying for is….can Tucker’s lungs handle the poking/prodding and invasion of surgery. Please pray that he sails through.
Tracheoesophogeal Fistula Repair- This will be the first thing they check. It’s still unclear on whether or not there is actually a connection between the trachea and the esophagus. If there is one, they will ligate the fistula. It’s also unknown if they’ll be able to repair it through a thoracotomy or if they’ll need to make a different incision through his neck.They ended up classifying this as a diverticulum instead of a TE Fistula…but they felt that it was large enough that it should be repaired. Sounds like they made an incision through the neck for this ligation.
- Esophagus Connection- The main goal of the surgery is to work towards an esophagus connection. His esophagus needs to be connected so that he is able to eat food AND to ensure that he doesn’t aspirate from his own secretions/saliva so that his lungs can finally begin to heal. It’s unknown if the two parts of his esophagus will stretch together easily or not. So there’s different ways that this will turn out;
Direct Anastomosis. It’s possible that as soon as they disect the esophagus away from the trachea that the two ends will easily stretch to one another and are able to be sewn them together.Internal Traction. If it’s too tight of a stretch and just needs a little more length, they will suture each end and pin it down to the rib. After a week or so, the ends have relaxed into position, grown a little, and then they are able to do an anastomosis to join them together.- External Traction. The ends may not come together at all and they will need to grow the ends together. This technique is called the Foker procedure. They’ll suture each end, draw them out through their incision and place it under tension. Every few days, they will increase the tension allowing the ends to grow towards one another. Once there’s enough overlap, they’ll go back in and connect it.
Internal and External Traction. Another option may even be a combination of both.
- Diaphragm Plication- After a visual inspection of the diaphragm, they may decide to do a diaphragm plication. This flattens out the diaphragm so that Tucker can take deeper breathes.
Wednesday, January 16, 2013
Tucker’s tracheostomy has been canceled for tomorrow.
{Yes, you did read that right}.
Instead, he will go to surgery on Friday for the “big surgery” to connect his esophagus and correct his fistula. A trach has been taken off of the table indefinitely.
Tommy and I both are still in disbelief; however, Tucker has been full of surprises since day one, and you might think as his parents we would “get it” by now.
Tucker’s pressure settings have come down to 18/6 today – those are the specific settings that Tucker’s team set as the benchmark to feel safe moving forward with his esophagus repair a couple of weeks ago.
Basically, Tucker has been cruising on the ventilator since Sunday night.
We don’t know why or how, but Tucker’s doctor said today that since “Tucker rose to the occasion,” we are going to take his lead and “go for it.”
The surgery will likely be the first one on the schedule for Friday and could take all day. (Think 7:30 am until dinner time). A few friends have expressed a desire to fast and pray alongside our family on Friday given the magnitude of this surgery for Tucker.
Here are a few specific prayer requests in preparation for Friday:
- The next 36 hours for Tucker need to be smooth and comfortable; that the Lord will be preparing his lungs and his body for a lengthy procedure on Friday, and that he won’t self-extubate or try anything crazy on us between now and Friday.
- For the surgeon’s ability to connect Tucker’s esophagus ends without having to put them under traction.
- If the surgeon is unable to do a primary connection on Friday and has to put Tucker under traction, that it will be the type of traction that is the least invasive and damaging to his lungs.
- The anesthesia team – that they would be wise and attuned to Tucker’s comfort level over the course of a lengthy surgery.
- Safety, skill, and discernment on the part of Tucker’s surgeons.
Friday’s surgery could be the game changer that allows him to eat and stops the aspirations that continue to cause damage to his lungs.
If the surgeons feel at any point that Tucker is not tolerating the operation, they will make the decision to pull out of the OR and wait until a later date to proceed with surgery. Pray that Tucker tolerates the operation like a champ and that they are able to achieve all that they hope to.
Here. We. GO.
Tuesday, January 15, 2013
We don’t want to get overly excited….but there’s a very small chance that we might have one other shot at avoiding a tracheostomy. The last few days Tucker has been doing great and they’ve been able to ween his pressures down to 20/7 (down from 26/8). They will likely ween him again tonight to 20/6 or possibly 18/6. What the doctors were hoping that Tucker could accomplish in 1 week appears to have taken him 2. OR time is still scheduled for Thursday but if the next 24 hours go swimmingly, we’d love to reengage in conversations about knocking out “the big surgery,” sooner rather later. We’re at peace with the idea of a trach but for obvious reasons would love to avoid it if we’re able and if it’s what’s best for T. We’re praying for continued healing/restoration of Tucker’s lungs in order to handle whichever surgery is headed his way….thanks for praying along with us.
Monday, January 14, 2013
Tucker hit the big six month mark yesterday, weighing in at 13 lbs 10 ounces. He’s in the 65th percentile (based off his adjusted age). We haven’t had a whole lot of activity the last few days because we are waiting until Thursday’s surgery before making any big changes. Tucker is still intubated and sedated, which is a bummer for his parents because we haven’t been able to hold him or get him out of the bed for the last week and a half.
Another Virginia momma with an EA (Esophageal Atresia) baby wrote a blog post in our honor about trachs on Friday. If you didn’t see this on Facebook, check it out here: http://savingisaac.com/?p=255 .
Friday, January 11, 2013
“Sweet pea
Apple of my eye
Don’t know when and I don’t know why
You’re the only reason I keep on coming home” ~ Amos Lee

Never when we started this journey six months ago did I anticipate that we would end up here.
But then again, so much of our last six months has been unexpected challenge after unexpected challenge. And we are confident that as He has done every step of the way, the Lord will equip us with the wisdom, grace, and courage to handle this when we thought we couldn’t.
Today we decided to move forward with a tracheostomy for Tucker. I hate the thought of a trach for all of the wrong reasons and embrace it for all of the right ones.
Ultimately, Tucker’s need for respiratory support on the ventilator this week made it abundantly clear that his lungs aren’t ready for an esophagus repair, but he can’t continue to hang out on CPAP through his nose for another three months. Tucker needs more ventilation than he can provide on his own, and a trach is the safest and most developmentally appropriate way to deliver that support over the long term. If his oxygen requirements didn’t say it, his lung x-rays did.
Tucker’s trach surgery is scheduled for next Thursday, January 17th. Before the surgeon puts in his trach, Tucker’s Esophageal Atresia surgeon will also reexamine his fistula to make sure it isn’t causing him to aspirate his saliva. If it is, he will fix the fistula before they place the trach.
After Tucker’s tracheostomy, Tucker’s medical team will set an arbitrary deadline for lung improvement (likely 8-10 weeks) before they reconsider the esophagus repair and diaphragm repair that he was supposed to have today.
That extends our time in Boston, but the benefit of a trach is that Tucker can come home on it. He couldn’t have come home on CPAP or a high flow nasal cannula, and we would have had to go through the whole oxygen and pressure weaning process all over again post-surgery just for him to come home.
Some of the downsides are that the trach may cause some speech delays and could potentially mean we will need in-home care for Tucker, something we never anticipated about bringing him back to Richmond. Plus it will not solve the risk of Tucker aspirating his saliva without an esophagus repair, but it should at least minimize it.
I think Tommy and I can both say with absolute conviction that this is the right choice for Tucker, even if it’s not the option we prayed for. We get excited about the thought of what kind of progress Tucker can make by getting the true respiratory support that he needs by way of a trach, and seeing how happy he will be when he is not working as hard to breathe on CPAP.
In the meantime, I am not kidding when I say this pretty much scares the crud out of me as a parent.
But as with all things “Tucker,” we press forward and follow his feisty, spirited, and (at times unconventional) lead.
Thursday, January 10, 2013
“From the end of the earth, will I call unto Thee, when my heart is overwhelmed: Lead me to the rock that is higher than I.” Psalm 61:2
Tucker has been on muscle relaxers for almost 24 hours. He seems really comfortable, but it is strange for us to see him so still. We hung out by his bedside this morning and I read to him, which is something I haven’t done since he was a little guy in his isolette. In some ways I feel like we are reliving our first two months of his life in the NICU.
The muscle relaxer has brought his ventilator settings down, but not at the pace the doctors had hoped for. His current pressures are 22/7 (a big improvement from 30/9 earlier in the week), but not low enough to where the surgeons feel comfortable operating. (18/5 or 20/6 is their preference).
The paralytic today is still considered a trial run to see how much taking Tucker “out of the picture” makes a difference in terms of his tolerating the ventilator. They will take him off of the paralytic at some point in the next 12 hours to make assessments and recommendations.
We are going to have some big decisions to make for Tucker over the next several days. There is a lot of debate over what is the best way to handle Tucker’s surgical course. Even with “cowboy surgeons” as Tucker’s pulmonalogist described them, the options range from risky to very risky given the condition of his lungs.
And ultimately, the buck stops at us. And our choice for our kid. And truthfully, the weight of that is overwhelming. Because half the time we are idiots and can’t even make concrete decisions for ourselves. We have been parents for six months. We are young and stupid. And he is so little and so innocent – the thought of doing wrong by him makes me sick to my stomach.
If you have kids and you are reading this, you know what I mean. When you love your child so much you can’t breathe – and your deepest desire is to just protect them. Have mercy.
A few prayer requests…
- Wisdom, perspective, and unity amongst Tucker’s doctors.
- The same for us.
- Safety and protection for Tucker.
- Peace when we finally arrive at a game plan.
Wednesday, January 9, 2013
Surgery is off the table for Friday. Although each day Tucker has been doing better, the pressure settings on his ventilator are just too high for the surgeons to feel comfortable with moving forward with surgery. During a thoracotomy (surgical maneuver to gain access to the lungs and esophagus), it’s typical for one of the lungs to collapse….that’s why it’s so important for Tucker’s lungs to be in tip-top shape before attempting to repair his trachea, esophagus, and/or diaphragm.
So the plan for the next 24 hours is this…put Tucker under paralysis and see how low we can get pressure settings when the ventilator is doing all the work for him. This will be a 24 hour test. If his lungs respond well and we take a major step forward to weening him down then doctors will revisit the idea of scheduling surgery in the weeks to come. If surgery is in sight, then doctors will have additional conversations about paralysis, sedation, and the best pre-op plan for T-man. If there’s not a significant decrease then there’s one other possible intervention that we could attempt before we are forced to get a trach.
Tucker is currently under paralysis (muscle relaxer if you will) right now and looks very comfortable and peaceful. His vent settings were down to 24 over 8 @ 60% Oxygen. Doctors are hoping that he can get down to 20 over 7 by morning. The surgeons mentioned today that they’d feel comfortable with surgery when Tucker gets to 18 over 5. Pray for us to be amazed by the miraculous response of his lungs. These are extremely ambitious goals for the short-term…but our God is BIG and He’s in the business of doing BIG things. Ultimately He’s in control.
Tuesday, January 8, 2013
Overall, today has been a better day than the last four days.
It seems like we finally have Tucker’s sedation to a point where he is more comfortable. (He hated having a breathing tube down his throat as a preemie, so you can imagine his reaction as a bigger, stronger, more developmentally appropriate little guy). This is one situation where Tucker’s feisty tendencies and his spunk are not to his favor. Poor fella. When we left the hospital tonight, he seemed exhausted, but relaxed.
His vent settings have come down a little. From 30/9 at 70% oxygen to 26/8 at 60% oxygen. Still not fantastic, but certainly an improvement from the last couple of days.
We are still taking things one day at a time in regards to surgery on Friday. It is highly likely that Tucker will be put on muscle relaxers tomorrow at some point. The esophagus surgery scheduled for Friday would require several days of paralysis postoperatively to let things heal, so the original plan was to just extend that on the front end. We will see what kind of effect that has on his ventilator settings tomorrow and Thursday.
This continues to be a stressful and overwhelming week but we are hanging in there. Thanks for all the prayers, text messages, Facebook messages and love you’ve sent our way. Although we aren’t able to always respond, we read every one!
Monday, January 7, 2013 – EVENING
Respiratory purgatory. Party of 3.
I try really hard not to cuss on this blog. Keep it clean and make my grandmother proud.
But man have I felt like cussing the last four days. So instead I just cuss in conversation with Tommy. (Sorry, babe).
As Tommy mentioned in the two posts below, we have had a rough four days. The original plan was to put Tucker back on the ventilator last Friday for “therapeutic purposes,” but that has landed us on higher ventilator settings than anyone imagined or that the surgeons are willing to operate with.
We met with Tucker’s full team again this afternoon and had a much different conversation than our meeting with them last Monday. Surgery for Friday is now contingent upon Tucker coming down on both his oxygen and pressures on his vent settings. The plan is to give him until Wednesday to do that on his own.
If Tucker is still requiring the same level of respiratory support from the vent by Wednesday as he is today, the doctors will “take him out of the picture” and by that they mean they will put Tucker under full medical paralysis instead of sedation.
Medical paralysis would mean the ventilator would do all of the breathing for Tucker in anticipation of surgery. If his vent settings continue to come down after he’s under paralysis, surgery could still take place on Friday, but whether it will address all three of the issues that they originally planned is still undefined.
A lot depends on the next four days. We are in between a rock and hard place with chronic lung disease from Tucker being premature and esophageal atresia with a (now identified fistula) that continues to cause damage to his lungs because he can breathe in his saliva.
We are feeling weary and discouraged for sure.
Monday, January 7, 2013
Quick update. Yesterday was still a little rough but we’re making some headway and it appears that we’re recouping some lung health. Nurses have made some incremental adjustments to Tucker’s sedation to keep him comfortable and relaxed. The respiratory therapists have also made some marginal adjustments to open up his lungs and allow the machine to do the work for him. His pressure settings are now at 30 over 9 and he’s been averaging around 60% oxygen. Doctors will potentially increase his PEEP and/or sedation to keep this forward momentum going. His last chest x-ray was significantly improved since the first one taken immediately following intubation. Our surgical team is back on today….so we should be able to have some discussions about if this weekend has altered our plan of action. We’re praying and trusting that this was still the right move and that it will prepare his lungs to be optimal for surgery.
Saturday, January 5, 2013
Well, Tucker’s intubated but it’s been a pretty rough 24 hours. Apparently, Tucker was a little harder of an intubation than reported from the OR team from last weeks bronchoscopy. Tucker ended up needing some pretty heavy drugs in order to tolerate having a tube shoved down his trachea. The intubation was made difficult most likely because he developed a tolerance to pain meds and sedatives when he was on such a high amount while younger. Also since he’s older now and more aware of what’s going on, he can put up quite the fight. His new endotracheal tube finally went in…..but we think during the process he may have swallowed quite a bit of secretions which has most likely caused a significant amount of inflammation within his lungs (pneumonitis). His prior CPAP settings of 7 @ 47%, quickly rose to 30 over 8 @ 80% within the first 24 hours. This has been the complete opposite effect that we were hoping/planning. Tucker’s respiratory settings have not been this high since he was still a tiny 30 week old and I’m not sure if we’ve ever seen a chest x-ray this bad. He’s now on several sedative drips to keep him calm/relaxed.
It seems as if he’s recovering from the initial damage to his lungs but we’re not even close to the respiratory settings that we were at just 29 hours ago, prior to the intubation. We’re planning on giving it through the weekend to see how things shape up. Pray that doctors/nurses are able to ween his pressure settings down, that his oxygen requirement decreases, and that we see significant change and improvement in his lungs within a very short amount of time. We are feeling like we’ve taken some major steps backwards and just days before a big surgery that’s supposed to move us forward. Surgery is contingent upon his lungs being in good shape…so this is all vitally important.
Thursday, January 3, 2013
Over the next 24 hours, we will see Tucker with two things that we have not missed the last three months: a PICC line (central IV line) and an endotrachial (breathing) tube….all in preparation for surgery next week, so these are good things. (They just bring back some not-so-fond memories of his prematurity for his parents).
We received an official date for Tucker’s surgery. It will take place next Friday, January 11th. No time yet, but we probably won’t know that until 24 hours beforehand. Because the surgical team is planning to address several issues at once, we also don’t know the length of the surgery. Likely, the surgeons won’t know until they get in there.
Sometime late today or early tomorrow, Tucker will be sedated and intubated. He will stay sedated and intubated for the next week prior to his surgery so that his medical team can better ventilate his lungs in preparation.
If you could pray for our hearts and for Tucker over the next few days that would be wonderful. Tucker’s pulmonologist mentioned that even with these surgeries (below), he still thinks there is a large chance Tucker will need a tracheostomy after the other issues are addressed because his lung disease is that severe from being born premature. We are trusting the Lord with Tucker’s health especially over the next few weeks, believing that the One who started a good work in Tucker will see it through to fruition.

Tuesday, January 1, 2013
Happy New Year! Tucker’s pulmonologist told us yesterday that “2013 is going to be the year for Tucker.” If you read our post from Saturday, you may remember that we were scheduled to have our big meeting with Tucker’s medical team tomorrow (Wednesday). Because the Esophageal Atresia team had an opportunity to meet yesterday (Monday) to discuss Tucker’s plan of action during the weekly clinical, we actually got our “game plan” earlier than we anticipated. We were anticipating a recommendation for a tracheostomy and then waiting several more months before his lungs are ready for the Foker procedure.
Prior to surgery, they want to intubate him for approximately one week and allow his lungs to become optimal for surgery. The surgeons will perform basically 4 procedures (our apologies for not knowing all the medical terminology for these specifics…..);
- Tracheoesophogeal Fistula Repair. It appears that there is an irregular connection between Tucker’s trachea (windpipe) and esophagus and the doctors will close off this connection.
- Tracheomalacia Repair. He has a fair amount of tracheomalacia and so the surgeons are going try and strengthen that on the posterior side as best they can.
- Diaphragm Repair. The fluoroscopy showed that his diaphragm wasn’t quite working symmetrically due to some “out-pouching” which makes it difficult for Tucker to take big deep breaths. The surgeons will pin that part of the diaphragm down.
- ESOPHAGUS REPAIR. Tucker’s gap appears to be about 3cm with a nice long distal stump. Surgeons are hoping that after they dissect out the fistula that they may be able to perform a direct anastomosis to simply connect the upper pouch to the distal stump. If it’s too far of a stretch they may put it under internal or external traction, allow it time to grow, and then go in again for a connection.
- A direct primary connection for Tucker would potentially eliminate the need for the Foker and potentially eliminate further trauma to his lungs and his airway by being intubated and for an extended period of time.
- Connecting Tucker’s esophagus and fixing his fistula reduces the opportunity for him to aspirate his saliva.
- We might actually see some lung improvement!

Saturday, December 29, 2012
We found out a few things yesterday from Tucker’s DLB and esophogram but we won’t find out the full details, possible plans for care, and/or our options for treatment until we meet with the full surgical team (most likely next Wednesday, January 2nd). Multiple parties need to review some of the imaging and weigh in on what they think is best for Tucker. Here are some of the things that have been confirmed thus far;
- Doctors saw what appeared to be a TE fistula in his upper esophageal pouch. There’s varying speculation on if it’s in fact a fistula (an irregular connection between the trachea and esophagus) or just a little pit/groove (diverticulum). So there’s question to how much this is currently impacting his respiratory status.
- Tucker has level 1 subepiglottic stenosis, which is a narrowing of his airway right below the epiglottis. This could be a result from him being intubated for the first couple months of his life.
- His airway is moderately floppy, tracheomalacia. The structure looks good but it’s fairly floppy.
- He has noticeable swelling and secretions throughout his trachea and esophagus.
- His distal esophageal stump has a good amount of length on it and Boston’s esophogram measured the distance between the upper pouch and the distal stump at 3.5 vertebral bodies (about 3cm). I believe this distance was measured without pushing on the ends and simply a contrast study. This is tremendous news because it puts us into the mild side of long-gap esophageal atresia. Knowing this new distance could alter and potentially simplify how the surgeons would like to proceed for his repair. We’ll wait and see.
In other news of Tucker, tests confirmed that he caught a little cold (rhinovirus) last week, so we were moved into an isolation room. He’s also on another short pulse of steroids and a lower CPAP of 7.
Friday, December 28, 2012 – 9:00 am. Initial results are back from Tucker’s bronchoscopy and laryngoscopy. The doctor found a high proximal fistula creating an irregular connection between his trachea and his esophagus, which explains why his lungs have continued to look wet. Basically, even with a replogle, there has been constant opportunity for Tucker to breathe in his saliva and “drown” his lungs. This explains the lack of respiratory improvement and the continued messy state of his lungs. This also means his surgeons may want to fix the fistula before considering a trach. We’re still waiting to hear from the team and have a more thorough conversation of what’s to come. Friday, December 28, 2012 – 5:00 am. If you think of it, say a prayer for Tucker-man this morning. He has a procedure scheduled for this morning in the operating room to examine his airway and determine whether he needs a trach. Additionally, they will do a gap-o-gram to give us a measurement of the gap between his stomach and upper esophagus. Appointment is scheduled for 7:30 am. We are en route to the hospital now. Thursday, December 27, 2012Our family left yesterday after a sweet five-day visit to Boston for Christmas. Ellie’s parents, “Grandad and Emi,” and Tucker’s Uncle Luke and Aunt Sarah Lynn drove from Richmond last Friday and spent the week with us exploring Boston and visiting Tucker. Unfortunately, Tucker got sick on Saturday with aspiration pneumonia (again – blerg). This meant he was pretty much down and out the entire time our family was here. They hadn’t seen Tucker in about a month, so we were really eager for them to have the opportunity to see how engaged and alert he is and some of the new developmental things he’s doing. Our attempt to take a family photo with Tucker face-planted on his boppy, Santa hat flopped down, and arms hanging over the front of the boppy pretty much sums up how Tucker was most of their visit. Fortunately, Tucker rallied (or the antiobiotics and steroids kicked in) Tuesday afternoon before they left so they did get to have one really good visit on Tuesday night where Tucker was acting much more like his happy, bright-eyed little self. A couple of updates:
- Tucker now weighs 11 lbs 7 ounces. Get after it, chunk.
- On Friday, December 28th, Tucker will have a bronchoscopy, and laryngoscopy and an esophagram. He will be put under anesthesia for this and intubated. The goal of the procedure is to examine Tucker’s airway and determine what kind of irregularities we might be dealing with related to his trachea and larynx. This procedure will be the determining factor as to whether or not Tucker gets a tracheostomy, so we sure would appreciate your prayers tomorrow (Friday).


 Tuesday, December 25, 2012 Merry Christmas from our family to yours!
Tuesday, December 25, 2012 Merry Christmas from our family to yours!  Monday, December 24, 2012
Monday, December 24, 2012
Wednesday, December 19, 2012
Our little turkey has now reached butterball status. He hit the 10 lb mark on Monday (10 lbs 6 ounces as of this morning). It is crazy to see fat rolls on our little guy, given how tiny and fragile he was when he was born.
Still not much progress on Tucker’s respiratory status, which has been pretty discouraging given that his esophagus surgery rides upon his lung status. Although his esophagus surgery was initially scheduled for mid-January, we still don’t have a date or concrete plans because of the lack of lung improvement.
Right now, Tucker is actually requiring more respiratory support than when we arrived here in Boston. (When we came on November 26th, Tucker was on a high flow nasal cannula and they transitioned him to CPAP after a couple days of being here).
Yesterday, Tucker went up again on his CPAP pressures from 7 to 8, which is the highest pressure Boston allows before they reintubate a baby and put them back on a ventilator. Ugh.
Tucker’s medical team is in the process of scheduling him for several diagnostic studies: a “gap-o-gram” or an esophagram to measure the length of Tucker’s esophageal gap and a bronchoscopy to look at Tucker’s airway and determine whether there are any irregularities that are affecting his ability to breathe.
On Thursday of last week, Tucker’s neonatologist brought up a possibility that I have been dreading and praying against for months – a tracheostomy. He told us that given Tucker’s gestational age (47 weeks), this is the point at which he starts to consider giving a baby a trach if the baby is still requiring CPAP and can’t get off.
Tommy is in a better place than I am about the possibility of a tracheostomy. I am still hating it…hating it, hating it.
There are more conversations still to be had before we have a larger conversation about Tucker’s surgical plan. We are praying for respiratory progress, wisdom for the doctors, and unity as parents in terms of how to best care for our child.
There are many moments along this journey where I think, “We are too young, too ill-equipped, too ignorant to have to make these kind of decisions for our child.”
But if not us, then who?
Sunday, December 16, 2012
Meet Mr. Tapeface.

This picture was taken yesterday (Saturday) and captures the look of “what the heck are you guys doing to me?” that we’ve seen on Tucker’s face the last four days.
Tucker has had a rough four days since our last entry. Nothing terrible – no “nose dives” on the respiratory front, but on Thursday, Tucker started gagging and coughing on his replogle tube like we have never seen. Poor fella. Eyes rolling back in his head gagging. It was distressing to watch for us, and for his nurses.
When he was asleep, he was okay – but when he was awake, he was angry, tonguing his replogle tube out of his mouth and just acting generally frustrated and mad at life.
We aren’t sure why, after five months of having a replogle down his throat, Tucker has developed a terrible aversion – perhaps it’s developmental. Yesterday, his medical team decided to add a “second replogle” to his face by threading the suction tube through his nose and down his throat into his esophageal pouch.
To make a long story short, having two replogles just made Tucker more upset and after another bumpy night (last night) of Tucker being upset and over-tired, the attending made the decision to pull the replogle out of Tucker’s mouth and just keep one replogle tube in his nose.
Tucker seems a whole lot more comfortable today, and – for the first time in five months – his little mouth is apparatus-free. Meaning he can cough, suck on his pacifier, and his parents can admire his sweet, unobstructed double chin.
Here’s our guy, all tuckered out after four days of trying to tell us he was done with having a suction tube in his mouth.

Tuesday, December 11, 2012
Our sweet and talented sister-in-law, Sarah took some “newborn” photos of Mr. Tucker before we left Richmond in November. More photos to come, but here is a little preview of her beautiful work. Thanks, Aunt Sarah. We love you!

Sunday, December 9, 2012
A friend asked me the other day how I liked being a parent. My typical answer to this question is something to the effect of, “Well, we haven’t had the most traditional entry into parenthood….”
Then another friend from high school stopped by Boston Children’s yesterday and asked me if we had any idea, when Tucker was born, that so many people would follow his story on our blog.
And I was struck with this deep sense of gratitude for our child. That he was given to us to take care of and provide for, to be stewards of his little life. Sometimes I think we get so caught up in the day to day, in-and-out routine of his medical journey that we forget he is a living and breathing miracle.
I am not going to romanticize the last four months and say that Tucker’s course has been a sweet “adventure” – Tucker’s first two months of life were probably the darkest months of our lives.
But getting to see how far he has come and watching his little personality develop…those are the moments where I feel the most like a parent.
Tucker is incredible. He loves people. He has the biggest, brightest eyes I’ve ever seen on a baby, and he is interested in everything. He is feisty and stubborn, but he’s also pretty happy and sweet-natured.
His strength and resilience humble me on a daily basis.
Saturday, December 8, 2012
Tucker’s last few days have been non-eventful which is both a good and not great thing. I think we all (including his medical team and surgeon) would like Tucker to be making a little more progress in terms of weaning his oxygen and CPAP pressures. His team tried weaning his CPAP from 7 to 6 a couple of times this week and they ended up moving him back up to 7 because they felt like he was having more desats and requiring more oxygen.
All that to say, we are certainly not in dire straits on respiratory end, but we also are not gaining a ton a traction. He was actually on less oxygen support when we were back home in Richmond, so we aren’t sure why – with a prolonged course of steroids here in Boston, that not much change has taken place.
There are a couple of other questions as to why Tucker’s respiratory improvement has been so slow, mostly having to do with his esophagus and his airway.
- The EMT who helped transfer Tucker from Richmond described his esophagus as a “spit pit,” which I guess is an easy way of describing it. Tucker’s throat basically ends below his neck in a blind pouch. Because Tucker’s esophagus is not attached to his stomach, he cannot swallow spit into his stomach like someone with a normal esophagus. Although he has the replogle (suction catheter) in his mouth running at continuous suction all the time, there is always the risk of “micro aspirations” – meaning that there’s always the risk of Tucker breathing in saliva and adding fluid to already damaged premature lungs.
- Kids who have esophageal atresia tend to also have an irregular airway, and some degree of tracheomalachia, or a “soft windpipe.” What degree of tracheomalachia Tucker has still needs to be explored, but it could be a contributing factor to his lack of respiratory progress as well.
- Chronic lung disease in former preemies like Tucker can also take 2 – 3 years (yes, years!) for a child to outgrow. Basically it’s a waiting game for a child’s healthy lung tissue to outweigh their damaged lung tissue from being on the ventilator for so long.
All that to say, Tucker’s respiratory course is complicated. Doctors here feel like Tucker’s lungs still aren’t in good enough shape for the Foker method, but we are all asking to what degree is his un-fixed esophagus preventing lung progress?
Here’s a picture of what Tucker’s esophagus currently looks like. Doctor’s believe Tucker has Isolated EA 1 (the image second to the right below).
Wednesday, December 5, 2012
This past weekend, Tommy and I traveled home to Virginia to be with our Young Life kids on Fall Weekend at Rockbridge. Tucker was in great hands the entire weekend and apparently had lots of visitors and attention from some sweet volunteers who came and held him while we were gone.
When we returned to Boston late Sunday night, he had a mirror, a mobile, and a cd player next to his bedside. According to his nurses, he loved watching himself in the mirror the entire weekend. And he loves music, too.
Boston has been very pleased with where Tucker is developmentally, which is a huge reassurance to us as parents.
Until Tucker is about 2 or 3 years old, his development will be measured by his adjusted age because he was born so prematurely. So in our language, even though Tucker has been with us since July, he is technically five and a half weeks old according to his October 21st due date.
Developmentally, he has already ticked off a bunch of three month old milestones….he tracks with his eyes, pushes with his legs, has good head and neck control. Strong physically and very feisty. His nurses also talk about how social and inquisitive he is, as evidenced by the little video we took below:
On the respiratory front, Tucker is is the “smoothest” we have ever seen him. Very few desats, good blood gases. Tucker is still on CPAP (which is a higher level of respiratory support than the nasal cannula has was on in Richmond); however, his doctors are taking things slow. He is now on a daily course of steroids which also seems to be helping with lung improvement.
We mentioned last week that Boston wanted to do a full “VACTERL” work-up on Tucker to check for the other midline birth defects that can be associated with Tucker’s arm and esophagus abnormalities. His echocardiogram came back normal (which wasn’t new news to us, but certainly nice to hear Boston’s affirmation that his heart is normal/healthy).
Other than that, we are settling into life in Boston. We are loving the family we are living with, and adjusting to our commute through Boston traffic….which we have learned in Boston, it’s pretty much “eat or be eaten” on the road.
Monday, December 3, 2012
Happy December! Our little nugget had a good first weekend in Boston. More details to come on Tuesday. Friday, November 30, 2012 It’s been a busy first week for Tucker in Boston. As we mentioned on Tuesday, Tucker’s team is spending a lot of time getting to know him and establishing a baseline for his respiratory care. They are also doing a full “VACTERL” work-up on Tucker to check him for the other midline defects that are commonly associated with Tucker’s esophageal atresia and radial aplasia. Boston sees a good number of VACTERL association kids, so we are interested in their perspective on Tucker’s birth defects. So far, Tucker has had an echocardiogram and a renal ultrasound done. Kidneys look perfectly normal, which is great! We haven’t heard their take on his echocardiogram yet, but his past echos have been good so hopefully that will stand true. On the respiratory front, Tucker’s neonatologist (who is also a pulmonalogist who specializes in premature lung disease) decided to go ahead and put Tucker on a prolonged course of steroids to get his lungs ready for surgery. We are hoping that this will bring his oxygen requirements down and lessen his need for respiratory support. In other news, Tucker was fitted yesterday for a “cranial cup,” which is something being developed for babies born prematurely with some head molding that has taken place. Since Tucker was born early and has spent a lot of time in a hospital bed, his head has taken on some narrowing on the sides. This cranial cup (different from a head helmet) is essentially a foam bed custom fitted to help round out the back of Tucker’s head. Pretty neat, and the nurses say that they have really seen good results with it. Last bit of news is that we met with Tucker’s medical team and his surgical team, and the consensus is that as of right now, surgery definitely will not take place before the end of 2012. Likely, early January 2013. Tuesday, November 27, 2012 Tucker’s first full day in Boston went well. He is settling into his new home, and I am pretty sure his parents are more overwhelmed than he is. Right now, his doctors and nurses are focusing on establishing a baseline for his respiratory course here before they are able to move on to surgery to repair Tucker’s esophagus. Since Tucker’s oxygen requirements were up from the day prior and his C02 was relatively high (in the 70s) on his blood gas, the neonatologist decided to go ahead and put Tucker back on CPAP to provide a little more respiratory support than the high-flow cannula in hopes of opening his lungs back up. Tucker also now has a separate probe that measures his C02 level (moment-by-moment) which matches his baseline blood gas they drew earlier. This way, his medical team can watch and see if his CO2 level is trending down to where they want (in the 50s – 60s). If putting Tucker back on CPAP does not bring his CO2 or oxygen requirements down, his team may consider another dose of steroids. Tucker also has a new protocol for his replogle (suction catheter) that goes down his throat and keeps secretions (saliva) out of his airway since he can’t swallow his spit into his stomach. Boston has replogles that are designed specifically for children with Esophageal Atresia, made to go down into Tucker’s esophageal pouch. They run Tucker’s replogle on continuous suction. Pretty cool (and the suction noise is strangely quiet, which is new for us). Although we are impressed by Boston Children’s, we definitely miss the warmth and familiarity of our NICU back in Richmond. To see a few images from our last 36 hours, check out our friend Kyle’s blog:  Monday, November 26, 2012 BOSTON. We are here! (After what was probably one of the longest days of our lives). Tucker’s transport went smoothly. We left Richmond around 1 pm and arrived in Boston around 3:30 pm. Tucker kept it classy by flying on an eight passenger jet which felt no wider than our Toyota minivan and about as long as a sailboat. The plane was tiny! Tucker sucked on his wubanub pacifier the whole flight, and as long as he was sucking on his binky, he was a happy camper. His arrival at Children’s was a little overwhelming for all three of us, as we met a new team of nurses, doctors, social workers, surgeons, and other staff who will be taking care of our dude. With a transfer comes new protocols, new equipment, new faces, and I think by the end of the day Tucker, Tommy, myself, and Tucker’s new nurses were exhausted. We will continue to settle in tomorrow and give a more detailed update, with a few pictures from today’s adventures. In the meantime, here’s a pic of our favorite guy before he left Henrico Doctor’s in Richmond.
Monday, November 26, 2012 BOSTON. We are here! (After what was probably one of the longest days of our lives). Tucker’s transport went smoothly. We left Richmond around 1 pm and arrived in Boston around 3:30 pm. Tucker kept it classy by flying on an eight passenger jet which felt no wider than our Toyota minivan and about as long as a sailboat. The plane was tiny! Tucker sucked on his wubanub pacifier the whole flight, and as long as he was sucking on his binky, he was a happy camper. His arrival at Children’s was a little overwhelming for all three of us, as we met a new team of nurses, doctors, social workers, surgeons, and other staff who will be taking care of our dude. With a transfer comes new protocols, new equipment, new faces, and I think by the end of the day Tucker, Tommy, myself, and Tucker’s new nurses were exhausted. We will continue to settle in tomorrow and give a more detailed update, with a few pictures from today’s adventures. In the meantime, here’s a pic of our favorite guy before he left Henrico Doctor’s in Richmond.  Wednesday, November 21, 2012
Wednesday, November 21, 2012